User:Orachang/sandbox
Dental plaque is a biofilm or mass of bacteria that grows on surfaces within the mouth. It is a sticky colorless deposit at first, but when it forms tartar, it is often brown or pale yellow. It is commonly found between the teeth, on the front of teeth, behind teeth, on chewing surfaces, along the gumline, or below the gumline cervical margins.[1] Dental plaque is also known as microbial plaque, oral biofilm, dental biofilm, dental plaque biofilm or bacterial plaque biofilm.[1] While plaque is commonly associated with oral diseases such as dental caries (cavities) and periodontal diseases (gum diseases), its formation is a normal process that cannot be prevented.
Progression and build-up of dental plaque can give rise to tooth decay – the localised destruction of the tissues of the tooth by acid produced from the bacterial degradation of fermentable sugar – and periodontal problems such as gingivitis and periodontitis;[2] hence it is important to disrupt the mass of bacteria and remove it daily.[3] Removal of dental biofilm can prevent the development of caries and gum diseases.[3] Plaque control and removal can be achieved with correct tooth brushing and use of interdental aids such as dental floss and interdental brushes.[1]
Oral hygiene is important as dental biofilms may become acidic causing demineralization of the teeth (also known as dental caries) or harden into dental calculus (also known as tartar).[4] Calculus cannot be removed through tooth brushing or with interdental aids, but only through professional cleaning.[2]
Plaque formation[edit]
Dental plaque is a biofilm that attaches to tooth surfaces, restorations and prosthetic appliances (including dentures and bridges) if left undisturbed. Understanding the formation, composition and characteristics of plaque helps in its control.[5] An acquired pellicle is a layer of saliva that is composed of mainly glycoproteins and forms shortly after cleaning of the teeth or exposure of new teeth.[6] Bacteria then attach to the pellicle layer, form micro-colonies, and mature on the tooth, which can result in oral diseases. The following table provides a more detailed (six-step) explanation of biofilm formation:

Components of plaque[edit]
Different types of bacteria are normally present in the mouth. These bacteria, as well as leukocytes, neutrophils, macrophages, and lymphocytes, are part of the normal oral cavity and contribute to the individual's health.[1] Approximately 80–90% of the weight of plaque is water. While 70% of the dry weight is bacteria, the remaining 30% consists of polysaccharides and glycoproteins.[7]
Bacteria[edit]
The bulk of the microorganisms that form the biofilm are Streptococcus mutans and other anaerobes, though the precise composition varies by location in the mouth. Examples of such anaerobes include fusobacterium and actinobacteria.[1] S. mutans and other anaerobes are the initial colonisers of the tooth surface, and play a major role in the establishment of the early biofilm community.[8] These microorganisms are all naturally present in the oral cavity and are normally harmless. However, failure to remove plaque by regular tooth brushing means that they are allowed to proliferate unchecked and thereby build up in a thick layer, which can by virtue of their ordinary metabolism cause any of various dental diseases for the host. Those microorganisms nearest the tooth surface typically obtain energy by fermenting dietary sucrose; it is during fermentation that they begin to produce acids.
The bacterial equilibrium position varies at different stages of formation. Below is a summary of the bacteria that may be present during the phases of plaque maturation.
- Early biofilm: primarily Gram-positive cocci
- Older biofilm (3–4 days): increased numbers of filaments and fusiforms
- 4–9 days undisturbed: more complex flora with rods, filamentous forms
- 7–14 days: Vibrio species, spirochetes, more Gram-negative organisms[9]
Supragingival biofilm[edit]
Supragingival biofilm is dental plaque that forms above the gums, controlled over by Gram-positive bacteria[10]. It is the first kind of plaque to form after the brushing of the teeth. It commonly forms in between the teeth, in the pits and grooves of the teeth and along the gums. It is made up of mostly aerobic bacteria, meaning these bacteria need oxygen to survive. As plaque remains on the tooth for a longer period of time, anaerobic bacteria begin to grow in this plaque.[5]
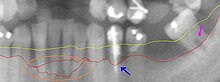
Subgingival biofilm[edit]

Subgingival biofilm is plaque that is located under the gums. It occurs after the formation of the supragingival biofilm by a downward growth of the bacteria from above the gums to below. This plaque is mostly made up of anaerobic bacteria, meaning that these bacteria will only survive if there is no oxygen. As this plaque attaches in a pocket under the gums, they are not exposed to oxygen in the mouth and will therefore thrive if not removed.[9]
The extracellular matrix contains proteins, long-chain polysaccharides and lipids.
The most common reasons for ecosystem disruption are the ecological factors discussed in the environment section. The bacteria that exhibit the most fit plasticity for the change in environment dominate the given environment. Often, this leads to opportunistic pathogens which may cause dental caries and periodontal disease. Pathogenic bacteria that have the potential to cause dental caries flourish in acidic environments; those that have the potential to cause periodontal disease flourish in a slightly alkaline environment.[11][failed verification]
Environment[edit]
The mouth is a warm and moist environment that is able to support the growth and development of dental plaque.[12] The main ecological factors that contribute to plaque formation are pH, saliva, temperature and redox reactions.[13][14] The normal pH range of saliva is between 6 and 7 and plaque biofilm is known to flourish in a pH between 6.7 and 8.3.[15][16] This indicates that the natural environment of the mouth provided by saliva is ideal for the growth of bacteria in the dental plaque. Saliva acts as a buffer, which helps to maintain the pH in the mouth between 6 and 7.[13] In addition to acting as a buffer, saliva and gingival crevicular fluid contain primary nutrients including amino acids, proteins and glycoproteins. This feeds the bacteria involved in plaque formation. The host diet plays only a minor role in providing nutrients for the resident microflora.[12] The normal temperature of the mouth ranges between 35 and 36 °C, and a two-degree (°C) change has been shown to drastically shift the dominant species in the plaque.[14] Redox reactions are carried out by aerobic bacteria. This keeps the oxygen levels in the mouth at a semi-stable homeostatic condition, which allows the bacteria to survive.[14]
Consequences of plaque build-up[edit]
Gingivitis[edit]

Gingivitis is a common result of plaque build-up around the gingival tissues. The bacteria found in the biofilm elicit a host response resulting in localized inflammation of the tissue.[17] This is characterized by the cardinal signs of inflammation including a red, puffy appearance of the gums and bleeding due to brushing or flossing.[18] Gingivitis due to plaque can be reversible by removal of the plaque. However, if left for an extended period of time, the inflammation may begin to affect the supporting tissues, in a progression referred to as periodontitis.[19] The gingivitis response is a protective mechanism, averting periodontitis in many cases.
Periodontitis[edit]
Periodontitis is an infection of the gums which leads to bone destruction around the teeth in the jaw. Periodontitis occurs after gingivitis has been established, but not all individuals who have gingivitis will get periodontitis.[20][21] Plaque accumulation is vital in the progression of periodontitis as the bacteria in plaque release enzymes which attack the bone and cause it to break down, and at the same time osteoclasts in the bone break down the bone as a way to prevent further infection. This can be treated with strict oral hygiene such as tooth brushing and cleaning in between the teeth as well as surgical debridement completed by a dental professional.[22]Piero Protect is a take home treatment that combines use of dental trays to hold a gel of hydrogen peroxide 1.7% W/W against the gums. Combined with regular plaque removal, it is possible that this home treatment can arrest the progress of the deterioration. Gum disease cannot be cured, but can be effectively treated, and can potentially assist to avoid surgery.
Caries[edit]

Dental caries is an infectious disease caused primarily by Streptococcus mutans, characterized by acid demineralization of the enamel, which can progress to further breakdown of the more organic, inner dental tissue (dentin).[1] Everybody is susceptible to caries but the probability of development depends on the patient’s individual disease indicators, risk factors and preventive factors. Factors that are considered high-risk for developing carious lesions on the teeth include:
- Low fluoride exposure
- Time, length, and frequency of sugar consumption
- Quality of tooth cleaning
- Fluctuations in salivary flow rates and composition
- Behavior of the individual
- Socioeconomic status of the individual
- Quality and composition of biofilms[1]
Organic acids released from dental plaque lead to demineralization of the adjacent tooth surface, and consequently to dental caries. Saliva is also unable to penetrate the build-up of plaque and thus cannot act to neutralize the acid produced by the bacteria and remineralize the tooth surface.
Detection of plaque build-up[edit]
There are two main methods of detecting dental plaque in the oral cavity: through the application of a disclosing gel or tablet, and/or visually through observation. Plaque detection is usually detected clinically by plaque disclosing agents. Disclosing agents contain dye which turns bright red to indicate plaque build-up.[1]
It is important for an individual to be aware of what to look for when doing a self-assessment for dental plaque. It is important to be aware that everyone has dental plaque, however, the severity of the build-up and the consequences of not removing the plaque can vary.[1]
Plaque disclosing gel[edit]

Plaque disclosing products, also known as disclosants, make plaque clinically visible. Clean surfaces of the teeth do not absorb the disclosant, only rough surfaces. Plaque disclosing gels can be either completed at home or in the dental clinic. Before using these at home or in the dental clinic check with your general practitioners for any allergies to iodine, food colouring or any other ingredients that may be present in these products. These gels provide a visual aid in assessing plaque biofilm presence and can also show the maturity of the dental plaque.
Disclosing tablets[edit]

Disclosing tablets are similar to that of disclosing gels, except that they are placed in the mouth and chewed on for approximately one minute. The remaining tablet or saliva is then spit out. Disclosing gels will show the presence of the plaque, but will often not show the level of maturity of the plaque. Disclosing tablets are often prescribed or given to patients with orthodontic appliances for use before and after tooth brushing to ensure optimal cleaning. These are also helpful educational tools for young children or patients that are struggling to remove dental plaque in certain areas. Disclosing gels and tablets are useful for individuals of all ages in ensuring efficient dental plaque removal.
Visual or tactile detection[edit]
Dental biofilm begins to form on the tooth only minutes after brushing. It can be difficult to visualise dental plaque on the hard tissue surfaces, however, a rough surface can be felt after eating or before tooth brushing if there is a thick deposit of dental plaque. It is often felt as a thick, fur-like deposit that may present as a yellow, tan or brown stain. They are commonly found on teeth or dental appliances such as orthodontic brackets and the tongue. The most common way dental plaque is assessed is through dental assessment in the dental clinic where dental instruments are able to scrape up some plaque. The most common areas where patients find plaque are between the teeth and along the cervical margins.
Plaque in dogs and cats[edit]
Dental plaque is also extremely common in domestic animals such as dogs and cats. However, the bacteria associated with canine and feline plaque appear to be different from that of humans.[23][24] If untreated it can lead to more severe gum disease such as periodontitis; hence veterinarians often recommend oral healthcare products for affected pets.
See also[edit]
References[edit]
- ^ a b c d e f g h i Darby M L, Walsh M M. Dental Hygiene Theory and Practice. 2010.
- ^ a b Wolf H and Hassell T (2006). Color Atlas of Dental Hygiene, Thieme New York, 333 Seventh Avenue, New York
- ^ a b Verkaik M, Busscher H, Jager D, Slomp A, Abbas F, van der Mei H. "Efficacy of natural antimicrobials in toothpaste formulations against oral biofilms in vitro". Journal of Dentistry. 2011;39(3):218–24.
- ^ James B. Summitt (2006). J. William Robbins, Thomas J. Hilton, Richard S. Schwartz, Jose Dos Santos Jr. (ed.). Fundamentals of Operative Dentistry: A Contemporary Approach. ISBN 978-0867154528.
{{cite book}}: CS1 maint: multiple names: editors list (link) - ^ a b Chetrus V and Ion I.R (2013). "Dental Plaque – Classification, Formation, and Identification." Int. J. Med. Dentistry 3: 139–43.
- ^ Kreth, Jens; Merritt, J.; Qi, F. (August 2009). "Bacterial and Host Interactions of Oral Streptococci". DNA and Cell Biology. 28 (8). Mary Ann Liebert, Inc.: 397–403. doi:10.1089/dna.2009.0868. PMC 2903342. PMID 19435424. Retrieved 2012-08-22.
{{cite journal}}: Unknown parameter|subscription=ignored (|url-access=suggested) (help) - ^ P D Marsh, D J Bradshaw. "Dental plaque as a biofilm." Journal of Industrial Microbiology. 1995. Volume 15. Number 3. p. 169.
- ^ Kolenbrander P. "Oral Microbial Communities: Biofilms, Interactions, and Genetic Systems" 1. Annu Rev Microbiol. 2000; 54(1):413–37.
- ^ a b Wilkins E. Clinical Practice of the Dental Hygienist. Philadelphia: Wolters Kluwer Health/Lippincott Williams & Wilkins; 2009
- ^ STRUŻYCKA, IZABELA (1 February 2014). "The Oral Microbiome in Dental Caries". Polish Journal of Microbiology. 63 (2): 127–135. doi:10.33073/pjm-2014-018. PMID 25115106.
- ^ Garcia, F.; Hicks, M.J. (May 2008). "Maintaining the Integrity of the Enamel Surface: The role of dental biofilm, saliva, and preventative agents in the enamel demineralization and remineralization". Journal of the American Dental Association. 139 (suppl. 2). American Dental Association: 25S–34S. doi:10.14219/jada.archive.2008.0352. PMID 18460677.
- ^ a b Marsh PD, Moter A, Devine DA. (2011). "Dental plaque biofilms: communities, conflict, and control". Periodontology 2000. 55(1), 16–35.
- ^ a b Marsh, P.D. (February 2003). "Are dental diseases examples of ecological catastrophes?". Microbiology. 143 (2). Society for General Microbiology: 279–94. doi:10.1099/mic.0.26082-0. PMID 12624191. Retrieved 2012-08-22.
- ^ a b c Marsh, P.D.; Devine, D.A. (February 2011). "How is the development of dental biofilms influenced by the host?". Journal of Clinical Periodontology. 38 (s11). John Wiley & Sons: 28–35. doi:10.1111/j.1600-051X.2010.01673.x. PMID 21323701. Retrieved 2012-08-22.
- ^ Humphrey, S. P., & Williamson, R. T. (2001). A review of saliva: normal composition, flow, and function. The Journal of prosthetic dentistry, 85(2), 162–69.
- ^ McDermid A, McKee A, Marsh P. "Effect of Environmental pH on Enzyme Activity and Growth of Bacteroides gingivalis W50". Infection and Immunity. 1998; 56(5):1096–100.
- ^ The American Academy of Periodontology. Proceedings of the World Workshop in Clinical Periodontics. Chicago:The American Academy of Periodontology; 1989:I/23-I/24.
- ^ Parakrama Chandrasoma, Clive R. Taylor (c. 2005). "Part A. General Pathology, Section II. The Host Response to Injury, Chapter 3. The Acute Inflammatory Response, sub-section Cardinal Clinical Signs". Concise Pathology (3rd edition (Computer file) ed.). New York, N.Y.: McGraw-Hill. ISBN 0-8385-1499-5. OCLC 150148447. Retrieved 2008-11-05.
- ^ Noble SL. Clinical Textbook of Dental Hygiene and Therapy, 2nd ed. West Sussex, Wiley-Blackwell; 2012. pp. 96–97.
- ^ Noble SL. Clinical Textbook of Dental Hygiene and Therapy, 2nd ed. West Sussex, Wiley-Blackwell; 2012. p. 111.
- ^ Rateitschak KH, Rateitschak EM, Wolf HF, Hassell TM. Color Atlas of Periodontology, New York, Thieme Inc; 1985. p. 55
- ^ Tonetti M S, Eickholz P, Loos B G, Papapanou P, van der Velden U, Armitage G, Bouchard P, Deinzer R, Dietrich T, Hughes F, Kocher T, Lang N P, Lopez R, Needleman I, Newton T, Nibali L, Pretzl B, Ramseier C, Sanz-Sanchez I, Schlagenhauf U, Suvan J E, Fabrikant E, Fundak A. "Principles in Prevention of Periodontal Diseases". Journal of Clinical Periodontology 2015, http://onlinelibrary.wiley.com/doi/10.1111/jcpe.12368/full?justLoggedIn=true&rememberMePresent=false.
- ^ The feline oral microbiome: A provisional 16S rRNA gene based taxonomy with full-length reference sequences. Floyd E. Dewhirsta, Erin A. Klein, Marie-Louise Bennett, Julie M. Croft, Stephen J. Harris, Zoe V. Marshall-Jones. Journal of Veterinary Microbiology, Volume 175, Issues 2–4, 25 February 2015, pp 294–303
- ^ Dewhirst FE, Klein EA, Thompson EC, Blanton JM, Chen T, Milella L, et al. (2012) The Canine Oral Microbiome. PLoS ONE 7(4): e36067.
