User:Mr. Ibrahem/Pancreatitis
| Pancreatitis | |
|---|---|
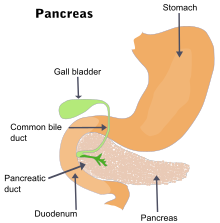 | |
| The pancreas and surrounding organs | |
| Specialty | Gastroenterology, general surgery |
| Symptoms | Pain in the upper abdomen, nausea, vomiting, fever, fatty stool[1] |
| Complications | Infection, bleeding, diabetes mellitus[1] |
| Duration | Short or long term[1] |
| Causes | Gallstones, heavy alcohol use, direct trauma, certain medications, mumps[1] |
| Risk factors | Smoking[2][3] |
| Diagnostic method | Based on symptoms, blood amylase or lipase[4][1] |
| Treatment | Intravenous fluids, pain medication, antibiotics[1] |
| Frequency | 8.9 million (2015)[5] |
| Deaths | 132,700 (2015)[6] |
Pancreatitis is a condition characterized by inflammation of the pancreas.[1] The pancreas is a large organ behind the stomach that produces digestive enzymes and a number of hormones.[1] There are two main types: acute pancreatitis, and chronic pancreatitis.[1] Signs and symptoms of pancreatitis include pain in the upper abdomen, nausea and vomiting.[1] The pain often goes into the back and is usually severe.[1] In acute pancreatitis, a fever may occur, and symptoms typically resolve in a few days.[1] In chronic pancreatitis weight loss, fatty stool, and diarrhea may occur.[1][4] Complications may include infection, bleeding, diabetes mellitus, or problems with other organs.[1]
The two most common causes of acute pancreatitis are a gallstone blocking the common bile duct after the pancreatic duct has joined; and heavy alcohol use.[1] Other causes include direct trauma, certain medications, infections such as mumps, and tumors.[1] Chronic pancreatitis may develop as a result of acute pancreatitis.[1] It is most commonly due to many years of heavy alcohol use.[1] Other causes include high levels of blood fats, high blood calcium, some medications, and certain genetic disorders, such as cystic fibrosis, among others.[1] Smoking increases the risk of both acute and chronic pancreatitis.[2][3] Diagnosis of acute pancreatitis is based on a threefold increase in the blood of either amylase or lipase.[1] In chronic pancreatitis, these tests may be normal.[1] Medical imaging such as ultrasound and CT scan may also be useful.[1]
Acute pancreatitis is usually treated with intravenous fluids, pain medication, and sometimes antibiotics.[1] Typically eating and drinking are disallowed, and a nasogastric tube is placed in the stomach.[1] A procedure known as an endoscopic retrograde cholangiopancreatography (ERCP) may be done to examine the distal common bile duct and remove a gallstone if present.[1] In those with gallstones the gallbladder is often also removed.[1] In chronic pancreatitis, in addition to the above, temporary feeding through a nasogastric tube may be used to provide adequate nutrition.[1] Long-term dietary changes and pancreatic enzyme replacement may be required.[1] And occasionally surgery is done to remove parts of the pancreas.[1]
Globally, in 2015 about 8.9 million cases of pancreatitis occurred.[5] This resulted in 132,700 deaths, up from 83,000 deaths in 1990.[6][7] Acute pancreatitis occurs in about 30 per 100,000 people a year.[2] New cases of chronic pancreatitis develop in about 8 per 100,000 people a year and currently affect about 50 per 100,000 people in the United States.[8] It is more common in men than women.[1] Often chronic pancreatitis starts between the ages of 30 and 40 while it is rare in children.[1] Acute pancreatitis was first described on autopsy in 1882 while chronic pancreatitis was first described in 1946.[8]
References[edit]
- ^ a b c d e f g h i j k l m n o p q r s t u v w x y z aa ab ac ad ae "Pancreatitis". niddk.nih.gov. August 16, 2012. Archived from the original on 7 March 2015. Retrieved 1 March 2015.
- ^ a b c Lankisch, PG; Apte, M; Banks, PA (20 January 2015). "Acute pancreatitis". Lancet. 386 (9988): 85–96. doi:10.1016/S0140-6736(14)60649-8. PMID 25616312.
- ^ a b Yadav, D; Lowenfels, AB (June 2013). "The epidemiology of pancreatitis and pancreatic cancer". Gastroenterology. 144 (6): 1252–61. doi:10.1053/j.gastro.2013.01.068. PMC 3662544. PMID 23622135.
- ^ a b Witt, Heiko (April 2007). "Chronic pancreatitis: challenges and advances in pathogenesis, genetics, diagnosis, and therapy". Gastroenterology. 132 (4): 1557–1573. doi:10.1053/j.gastro.2007.03.001. PMID 17466744.
- ^ a b GBD 2015 Disease and Injury Incidence and Prevalence, Collaborators. (8 October 2016). "Global, regional, and national incidence, prevalence, and years lived with disability for 310 diseases and injuries, 1990–2015: a systematic analysis for the Global Burden of Disease Study 2015". Lancet. 388 (10053): 1545–602. doi:10.1016/S0140-6736(16)31678-6. PMC 5055577. PMID 27733282.
{{cite journal}}:|first1=has generic name (help)CS1 maint: numeric names: authors list (link) - ^ a b GBD 2015 Mortality and Causes of Death, Collaborators. (8 October 2016). "Global, regional, and national life expectancy, all-cause mortality, and cause-specific mortality for 249 causes of death, 1980–2015: a systematic analysis for the Global Burden of Disease Study 2015". Lancet. 388 (10053): 1459–44. doi:10.1016/s0140-6736(16)31012-1. PMC 5388903. PMID 27733281.
{{cite journal}}:|first1=has generic name (help)CS1 maint: numeric names: authors list (link) - ^ GBD 2013 Mortality and Causes of Death, Collaborators (17 December 2014). "Global, regional, and national age-sex specific all-cause and cause-specific mortality for 240 causes of death, 1990–2013: a systematic analysis for the Global Burden of Disease Study 2013". Lancet. 385 (9963): 117–71. doi:10.1016/S0140-6736(14)61682-2. PMC 4340604. PMID 25530442.
{{cite journal}}:|first1=has generic name (help)CS1 maint: numeric names: authors list (link) - ^ a b Muniraj, T; Aslanian, HR; Farrell, J; Jamidar, PA (December 2014). "Chronic pancreatitis, a comprehensive review and update. Part I: epidemiology, etiology, risk factors, genetics, pathophysiology, and clinical features". Disease-a-month : DM. 60 (12): 530–50. doi:10.1016/j.disamonth.2014.11.002. PMID 25510320.
