Sarcopenia
| Sarcopenia | |
|---|---|
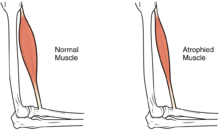 | |
| Difference between a normal muscle and an atrophied muscle | |
| Specialty | Geriatrics Rheumatology |
Sarcopenia (ICD-10-CM code M62.84[1]) is a type of muscle loss that occurs with aging and/or immobility. It is characterized by the degenerative loss of skeletal muscle mass, quality, and strength. The rate of muscle loss is dependent on exercise level, co-morbidities, nutrition and other factors. The muscle loss is related to changes in muscle synthesis signalling pathways. It is distinct from cachexia, in which muscle is degraded through cytokine-mediated degradation, although the two conditions may co-exist. Sarcopenia is considered a component of frailty syndrome.[2] Sarcopenia can lead to reduced quality of life, falls, fracture, and disability.[3][4]
Sarcopenia is a factor in changing body composition. When associated with aging populations, certain muscle regions are expected to be affected first, specifically the anterior thigh and abdominal muscles.[3][5] In population studies, body mass index (BMI) is seen to decrease in aging populations while bioelectrical impedance analysis (BIA) shows body fat proportion rising.[6]
A new sarcopenia related condition is the Steatosarcopenia proposed by the Steatosarcopenia & Sarcopenia Brazilian Study Group. This condition is characterized by the loss of mass or skeletal muscle strength and performance associated with the excessive deposition of ectopic reserve fat in muscle tissue, in the same individual, not necessarily related to [7]excess fat total body mass. Steatosarcopenia: A New Terminology for Clinical Conditions Related to Body Composition Classification.
Signs and symptoms
[edit]The hallmark sign of sarcopenia is loss of lean muscle mass, or muscle atrophy. The change in body composition may be difficult to detect due to obesity, changes in fat mass, or edema. Changes in weight, limb or waist circumference are not reliable indicators of muscle mass changes. Sarcopenia may also cause reduced strength, functional decline and increased risk of falling. Sarcopenia may also have no symptoms until it is severe and is often unrecognized.[2] Research has shown, however, that hypertrophy may occur in the upper parts of the body to compensate for this loss of lean muscle mass[3][8] Therefore, one early indicator of the onset of sarcopenia can be significant loss of muscle mass in the anterior thigh and abdominal muscles.[3]
Causes
[edit]There are many proposed causes of sarcopenia and it is likely the result of multiple interacting factors. Understanding of the causes of sarcopenia is incomplete, however changes in hormones, immobility, age-related muscle changes, nutrition and neurodegenerative changes have all been recognized as potential causative factors.[9]
The degree of sarcopenia is determined by two factors: the initial amount of muscle mass and the rate at which muscle mass declines. Due to variations in these factors across the population, the rate of progression and the threshold at which muscle loss becomes apparent is variable.[10] Immobility dramatically increases the rate of muscle loss, even in younger people. Other factors that can increase the rate of progression of sarcopenia include decreased nutrient intake, low physical activity, or chronic disease.[2] Additionally, epidemiological research has indicated that early environmental influences may have long-term effects on muscle health. For example, low birth weight, a marker of a poor early environment, is associated with reduced muscle mass and strength in adult life.[11][12][13]
Pathophysiology
[edit]There are multiple theories proposed to explain the mechanisms of muscle changes of sarcopenia including changes in myosatellite cell recruitment, changes in anabolic signalling, protein oxidation, inflammation, and developmental factors. The pathologic changes of sarcopenia include a reduction in muscle tissue quality as reflected in the replacement of muscle fibers with fat, an increase in fibrosis, changes in muscle metabolism, oxidative stress, and degeneration of the neuromuscular junction.[14] The failure to activate satellite cells upon injury or exercise is also thought to contribute to the pathophysiology of sarcopenia.[14] Additionally, oxidized proteins can lead to a buildup of lipofuscin and cross-linked proteins causing an accumulation of non-contractile material in the skeletal muscle and contribute to sarcopenic muscle.[10]
In sarcopenic muscle the distribution of the types of muscle fibers changes with a decrease in type II muscle fibers, or "fast twitch," with little to no decrease in type I muscle fibers, or "slow-twitch" muscle fibers. Deinervated type II fibers are often converted to type I fibers by reinnervation by slow type I fiber motor nerves.[15] Males are perhaps more susceptible for this aging-related switching of the myofiber type, as a recent research has shown a higher percentage of "slow twitch" muscle fibers in old compared to young males, but not in old compared to young females.[16]
Aging sarcopenic muscle shows an accumulation of mitochondrial DNA mutations, which has been demonstrated in various other cell types as well.[17] Clones with mitochondrial mutations build up in certain regions of the muscle, which goes along with an about fivefold increase in the absolute mtDNA copy number, that is, these regions are denser.[18] An apparent protective factor preventing cells' buildup of damaged mitochondria is sufficient levels of the protein BNIP3. Deficiency of BNIP3 leads to muscle inflammation and atrophy.[19]
Furthermore, not every muscle is as susceptible to the atrophic effects of aging. For example, in both humans[20] and mice[21] it has been shown that lower leg muscles are not as susceptible to aging as upper leg muscles. This could perhaps be explained by the differential distribution of myofiber type within each muscle group, but this is unknown.[citation needed]
Diagnosis
[edit]Multiple diagnostic criteria have been proposed by various expert groups and continues to be an area of research and debate. Despite the lack of a widely accepted definition, sarcopenia was assigned an ICD-10 code (M62.84) in 2016, recognizing it as a disease state.[22]
Sarcopenia can be diagnosed when a patient has muscle mass that is at least two standard deviations below the relevant population mean and has a slow walking speed.[23] The European Working Group on Sarcopenia in Older People (EWGSOP) developed a broad clinical definition for sarcopenia, designated as the presence of low muscle mass and either low muscular strength or low physical performance.[9] Other international groups have proposed criteria that include metrics on walking speed, distance walked in 6 minutes, or grip strength.[22] Hand grip strength alone has also been advocated as a clinical marker of sarcopenia that is simple and cost effective and has good predictive power, although it does not provide comprehensive information.[24]
There are screening tools for sarcopenia that assess patient reported difficulty in doing daily activities such as walking, climbing stairs or standing from a chair and have been shown to predict sarcopenia and poor functional outcomes.[25]
Biomarkers
[edit]As sarcopenia is a complex clinical diagnosis, circulating biomarkers have been proposed as proxies for early diagnosis and prediction as well as for follow-up and serial assessment of response to interventions.
Aging and sarcopenia are associated with an increase in inflammatory markers ("inflamm-aging") including: C-reactive protein, tumor necrosis factor, interleukin-8, interleukin-6, granulocyte-monocyte colony-stimulating factor, interferons, and serine protease A1.[26]
Changes in hormones associated with aging and sarcopenia include a reduction in the sex-hormones testosterone and dehydroepiandrosterone sulfate,[27] as well as reduced levels of circulating growth hormone and IGF-1.[28]
Circulating C-terminal agrin fragments (CAF) have been found to be higher in accelerated sarcopenic patients.[29]
Lower plasma levels of the amino acids leucine and isoleucine as well as other essential amino acids were found in frail older people compared to non-frail controls.[30][31]
Alanine aminotransferase (ALT) is responsible for the transfer of the α-amino group from an α-amino acid to an α-keto acid, transforming pyruvate to alanine in skeletal muscle. Low circulating ALT is a marker for low muscle mass and sarcopenia,[32] as well for increased disease activity in patients with inflammatory bowel disease.[33]
Management
[edit]Exercise
[edit]Exercise remains the intervention of choice for sarcopenia, but translation of research findings into clinical practice is challenging. The type, duration and intensity of exercise are variable between studies, preventing a standardized exercise prescription for sarcopenia.[34] Lack of exercise is a significant risk factor for sarcopenia and exercise can dramatically slow the rate of muscle loss.[35] Exercise can be an effective intervention because aging skeletal muscle retains the ability to synthesize proteins in response to short-term resistance exercise.[36] Progressive resistance training in older adults can improve physical performance (gait speed) and muscular strength.[37][38][39] Increased exercise can produce greater numbers of cellular mitochondria, increase capillary density, and increase the mass and strength of connective tissue.[40]
Medication
[edit]There are currently no approved medications for the treatment of sarcopenia.[41] Testosterone or other anabolic steroids have also been investigated for treatment of sarcopenia, and seem to have some positive effects on muscle strength and mass, but cause several side effects and raise concerns of prostate cancer in men and virilization in women.[42][43] Additionally, recent studies suggest testosterone treatments may induce adverse cardiovascular events.[44][45][46]
DHEA and human growth hormone have been shown to have little to no effect in this setting. Growth hormone increases muscle protein synthesis and increases muscle mass, but does not lead to gains in strength and function in most studies.[42] This, and the similar lack of efficacy of its effector insulin-like growth factor 1 (IGF-1), may be due to local resistance to IGF-1 in aging muscle, resulting from inflammation and other age changes.[42]
Other medications under investigation as possible treatments for sarcopenia include ghrelin, vitamin D, angiotensin converting enzyme inhibitors, and eicosapentaenoic acid.[42][43]
Nutrition
[edit]Intake of calories and protein are important stimuli for muscle protein synthesis.[47] Older adults may not utilize protein as efficiently as younger people and may require higher amounts to prevent muscle atrophy.[23] A number of expert groups have proposed an increase in dietary protein recommendations for older age groups to 1.0–1.2 g/kg body weight per day.[48][49] Ensuring adequate nutrition in older adults is of interest in the prevention of sarcopenia and frailty, since it is a simple, low-cost treatment approach without major side effects.[50]
Supplements
[edit]A component of sarcopenia is the loss of ability for aging skeletal muscle to respond to anabolic stimuli such as amino acids, especially at lower concentrations. However, aging muscle retains the ability of an anabolic response to protein or amino acids at larger doses. Supplementation with larger doses of amino acids, particularly leucine has been reported to counteract muscle loss with aging.[51] Exercise may work synergistically with amino acid supplementation.[41]
β-hydroxy β-methylbutyrate (HMB) is a metabolite of leucine that acts as a signalling molecule to stimulate protein synthesis.[23][41] It is reported to have multiple targets, including stimulating mTOR and decreasing proteasome expression. Its use to prevent the loss of lean body mass in older adults is consistently supported in clinical trials.[52][53][54] More research is needed to determine the precise effects of HMB on muscle strength and function in this age group.[53]
Epidemiology
[edit]The prevalence of sarcopenia depends on the definition used in each epidemiological study. Estimated prevalence in people between the ages of 60-70 is 5-13% and increases to 11-50% in people more than 80 years of age. This equates to >50 million people and is projected to affect >200 million in the next 40 years given the rising population of older adults.[9]
Public health impact
[edit]Sarcopenia is emerging as a major public health concern given the increased longevity of industrialized populations and growing geriatric population. Sarcopenia is a predictor of many adverse outcomes including increased disability, falls and mortality.[55][56] Immobility or bed rest in populations predisposed to sarcopenia can cause dramatic impact on functional outcomes. In the elderly, this often leads to decreased biological reserve and increased vulnerability to stressors known as the "frailty syndrome". Loss of lean body mass is also associated with increased risk of infection, decreased immunity, and poor wound healing. The weakness that accompanies muscle atrophy leads to higher risk of falls, fractures, physical disability, need for institutional care, reduced quality of life, increased mortality, and increased healthcare costs.[23] This represents a significant personal and societal burden and its public health impact is increasingly recognized.[9]
Etymology
[edit]The term sarcopenia stems from Greek σάρξ sarx, "flesh" and πενία penia, "poverty". This was first proposed by Rosenberg in 1989, who wrote that "there may be no single feature of age-related decline that could more dramatically affect ambulation, mobility, calorie intake, and overall nutrient intake and status, independence, breathing, etc".[citation needed]
Sarcopenia is distinct from cachexia, in which muscle is degraded through cytokine-mediated degradation, although the two conditions may co-exist.[citation needed]
Research directions
[edit]There are significant opportunities to better understand the causes and consequences of sarcopenia and help guide clinical care. This includes elucidation of the molecular and cellular mechanisms of sarcopenia, further refinement of reference populations by ethnic groups, validation of diagnostic criteria and clinical tools, as well as tracking of incidence of hospitalization admissions, morbidity, and mortality. Identification and research on potential therapeutic approaches and timing of interventions is also needed.[57]
As of 2020[update], there are no drugs approved to treat muscle wasting in people with chronic diseases, and there is therefore an unmet need for anabolic drugs with few side effects. One aspect hindering drug approval for treatments for cachexia and sarcopenia is disagreement in endpoints. Several clinical trials have found that selective androgen receptor modulators (SARMs) improve lean mass in humans, but it is not clear whether strength and physical function are also improved. After promising results in a phase II trial, a phase III trial of the SARM ostarine was proven to increase lean body mass but did not show significant improvement in function.[58] It and other drugs—such as the growth hormone secretagogue anamorelin—have been refused regulatory approval despite significant increases in lean mass due to a lack of evidence that they increased physical performance. Preventing decline in functionality was not considered an acceptable endpoint by the Food and Drug Administration. It is not known how SARMs interact with dietary protein intake and resistance training in people with muscle wasting.[59][60]
See also
[edit]- Ageing – Biological process of getting older
- Cachexia – Syndrome causing muscle loss not entirely reversible
- Dynapenia – Loss of muscular strength not caused by neurological or muscular disease
- Frailty syndrome – Weakness in elderly person
- Geriatrics – Specialty that focuses on health care of elderly people
References
[edit]- ^ Anker SD, Morley JE, von Haehling S (17 October 2016). "Welcome to the ICD-10 code for sarcopenia". Journal of Cachexia, Sarcopenia and Muscle. 7 (5): 512–514. doi:10.1002/jcsm.12147. ISSN 2190-5991. PMC 5114626. PMID 27891296.
- ^ a b c Peterson SJ, Mozer M (February 2017). "Differentiating Sarcopenia and Cachexia Among Patients With Cancer". Nutrition in Clinical Practice. 32 (1): 30–39. doi:10.1177/0884533616680354. PMID 28124947. S2CID 206555460.
- ^ a b c d Ata AM, Kara M, Kaymak B, Özçakar L (October 2020). "Sarcopenia Is Not "Love": You Have to Look Where You Lost it!". American Journal of Physical Medicine & Rehabilitation. 99 (10): e119–e120. doi:10.1097/PHM.0000000000001391. PMID 32084033. S2CID 211245329.
- ^ Beaudart C, Zaaria M, Pasleau F, Reginster JY, Bruyère O (2017). "Health Outcomes of Sarcopenia: A Systematic Review and Meta-Analysis". PLOS ONE. 12 (1): e0169548. Bibcode:2017PLoSO..1269548B. doi:10.1371/journal.pone.0169548. PMC 5240970. PMID 28095426.
- ^ Ata AM, Kara M, Kaymak B, Gürçay E, Çakır B, Ünlü H, et al. (2019). "Regional and total muscle mass, muscle strength and physical performance: The potential use of ultrasound imaging for sarcopenia". Archives of Gerontology and Geriatrics. 83: 55–60. doi:10.1016/j.archger.2019.03.014. PMID 30953961. S2CID 96463073.
- ^ Ranasinghe C, Gamage P, Katulanda P, Andraweera N, Thilakarathne S, Tharanga P (September 2013). "Relationship between Body Mass Index (BMI) and body fat percentage, estimated by bioelectrical impedance, in a group of Sri Lankan adults: a cross sectional study". BMC Public Health. 13: 797. doi:10.1186/1471-2458-13-797. PMC 3766672. PMID 24004464.
- ^ Michels G, Mattos Rosa G, Renke G, Starling-Soares B (November 2024). "Steatosarcopenia: A New Terminology for Clinical Conditions Related to Body Composition Classification". Life. 14 (11): 1383. doi:10.3390/life14111383. ISSN 2075-1729.
- ^ Özkal Ö, Kara M, Topuz S, Kaymak B, Bakı A, Özçakar L (November 2019). "Assessment of core and lower limb muscles for static/dynamic balance in the older people: An ultrasonographic study". Age and Ageing. 48 (6): 881–887. doi:10.1093/ageing/afz079. PMID 31268513.
- ^ a b c d Cruz-Jentoft AJ, Baeyens JP, Bauer JM, Boirie Y, Cederholm T, Landi F, et al. (July 2010). "Sarcopenia: European consensus on definition and diagnosis: Report of the European Working Group on Sarcopenia in Older People". Age and Ageing. 39 (4): 412–423. doi:10.1093/ageing/afq034. PMC 2886201. PMID 20392703.
- ^ a b Marcell TJ (October 2003). "Sarcopenia: causes, consequences, and preventions". The Journals of Gerontology. Series A, Biological Sciences and Medical Sciences (Review). 58 (10): M911–M916. doi:10.1093/gerona/58.10.m911. PMID 14570858.
- ^ Sayer AA, Syddall HE, Gilbody HJ, Dennison EM, Cooper C (September 2004). "Does sarcopenia originate in early life? Findings from the Hertfordshire cohort study". The Journals of Gerontology. Series A, Biological Sciences and Medical Sciences. 59 (9): M930–M934. doi:10.1093/gerona/59.9.M930. PMID 15472158.
- ^ Gale CR, Martyn CN, Kellingray S, Eastell R, Cooper C (January 2001). "Intrauterine programming of adult body composition". The Journal of Clinical Endocrinology and Metabolism. 86 (1): 267–272. doi:10.1210/jcem.86.1.7155. PMID 11232011.
- ^ Ylihärsilä H, Kajantie E, Osmond C, Forsén T, Barker DJ, Eriksson JG (September 2007). "Birth size, adult body composition and muscle strength in later life". International Journal of Obesity. 31 (9): 1392–1399. doi:10.1038/sj.ijo.0803612. PMID 17356523.
- ^ a b Ryall JG, Schertzer JD, Lynch GS (August 2008). "Cellular and molecular mechanisms underlying age-related skeletal muscle wasting and weakness". Biogerontology (Review). 9 (4): 213–228. doi:10.1007/s10522-008-9131-0. PMID 18299960. S2CID 8576449.
- ^ Doherty TJ (October 2003). "Invited review: Aging and sarcopenia". Journal of Applied Physiology (Review). 95 (4): 1717–1727. doi:10.1152/japplphysiol.00347.2003. PMID 12970377.
- ^ de Jong JC, Attema BJ, van der Hoek MD, Verschuren L, Caspers MP, Kleemann R, et al. (August 2023). "Sex differences in skeletal muscle-aging trajectory: same processes, but with a different ranking". GeroScience (Original Research). 45 (4): 2367–2386. doi:10.1007/s11357-023-00750-4. PMC 10651666. PMID 36820956.
- ^ Kauppila TE, Kauppila JH, Larsson NG (January 2017). "Mammalian Mitochondria and Aging: An Update". Cell Metabolism. 25 (1): 57–71. doi:10.1016/j.cmet.2016.09.017. PMID 28094012. S2CID 21609241.
- ^ Insalata F, Hoitzing H, Aryaman J, Jones NS (December 2022). "Stochastic survival of the densest and mitochondrial DNA clonal expansion in aging". Proceedings of the National Academy of Sciences of the United States of America. 119 (49): e2122073119. Bibcode:2022PNAS..11922073I. doi:10.1073/pnas.2122073119. PMC 9894218. PMID 36442091.
- ^ Irazoki A, Martinez-Vicente M, Aparicio P, Aris C, Alibakhshi E, Rubio-Valera M, et al. (April 2022). "Coordination of mitochondrial and lysosomal homeostasis mitigates inflammation and muscle atrophy during aging". Aging Cell. 21 (4): e13583. doi:10.1111/acel.13583. PMC 9009131. PMID 35263007.
- ^ Naruse M, Trappe S, Trappe TA (April 2023). "Human skeletal muscle-specific atrophy with aging: a comprehensive review". Journal of Applied Physiology (Original Research). 134 (4): 900–914. doi:10.1152/japplphysiol.00768.2022. PMC 10069966. PMID 36825643.
- ^ de Jong JC, Caspers MP, Worms N, Keijzer N, Kleemann R, Menke AL, et al. (June 2024). "Translatability of mouse muscle-aging for humans: the role of sex". GeroScience (Original Research). 46 (3): 3341–3360. doi:10.1007/s11357-024-01082-7. PMC 11009184. PMID 38265577.
- ^ a b Anker SD, Morley JE, von Haehling S (December 2016). "Welcome to the ICD-10 code for sarcopenia". Journal of Cachexia, Sarcopenia and Muscle. 7 (5): 512–514. doi:10.1002/jcsm.12147. PMC 5114626. PMID 27891296.
- ^ a b c d Argilés JM, Campos N, Lopez-Pedrosa JM, Rueda R, Rodriguez-Mañas L (September 2016). "Skeletal Muscle Regulates Metabolism via Interorgan Crosstalk: Roles in Health and Disease". Journal of the American Medical Directors Association. 17 (9): 789–796. doi:10.1016/j.jamda.2016.04.019. PMID 27324808.
- ^ Sayer AA (August 2010). "Sarcopenia". BMJ. 341 (aug10 2): c4097. doi:10.1136/bmj.c4097. PMID 20699307. S2CID 220113690.
- ^ Malmstrom TK, Miller DK, Simonsick EM, Ferrucci L, Morley JE (March 2016). "SARC-F: a symptom score to predict persons with sarcopenia at risk for poor functional outcomes". Journal of Cachexia, Sarcopenia and Muscle. 7 (1): 28–36. doi:10.1002/jcsm.12048. PMC 4799853. PMID 27066316.
- ^ Pan L, Xie W, Fu X, Lu W, Jin H, Lai J, et al. (October 2021). "Inflammation and sarcopenia: A focus on circulating inflammatory cytokines". Experimental Gerontology. 154: 111544. doi:10.1016/j.exger.2021.111544. PMID 34478826.
- ^ Shin MJ, Jeon YK, Kim IJ (September 2018). "Testosterone and Sarcopenia". The World Journal of Men's Health. 36 (3): 192–198. doi:10.5534/wjmh.180001. PMC 6119844. PMID 29756416.
- ^ Bartke A (January 2019). "Growth Hormone and Aging: Updated Review". The World Journal of Men's Health. 37 (1): 19–30. doi:10.5534/wjmh.180018. PMC 6305861. PMID 29756419.
- ^ Qaisar R, Karim A, Muhammad T, Shah I, Khan J (April 2021). "Prediction of sarcopenia using a battery of circulating biomarkers". Scientific Reports. 11 (1): 8632. doi:10.1038/s41598-021-87974-6. PMC 8060253. PMID 33883602.
- ^ Adav SS, Wang Y (April 2021). "Metabolomics Signatures of Aging: Recent Advances". Aging and Disease. 12 (2): 646–661. doi:10.14336/AD.2020.0909. PMC 7990359. PMID 33815888.
- ^ Calvani R, Picca A, Marini F, Biancolillo A, Gervasoni J, Persichilli S, et al. (November 2018). "A Distinct Pattern of Circulating Amino Acids Characterizes Older Persons with Physical Frailty and Sarcopenia: Results from the BIOSPHERE Study". Nutrients. 10 (11): 1691. doi:10.3390/nu10111691. PMC 6265849. PMID 30404172.
- ^ Portal D, Hofstetter L, Eshed I, Dan-Lantsman C, Sella T, Urban D, et al. (1 April 2019). "L3 skeletal muscle index (L3SMI) is a surrogate marker of sarcopenia and frailty in non-small cell lung cancer patients". Cancer Management and Research. 11: 2579–2588. doi:10.2147/CMAR.S195869. PMC 6497853. PMID 31114324.
- ^ Shafrir A, Katz LH, Shauly-Aharonov M, Zinger A, Safadi R, Stokar J, et al. (March 2024). "Low ALT Is Associated with IBD and Disease Activity: Results from a Nationwide Study". Journal of Clinical Medicine. 13 (7): 1869. doi:10.3390/jcm13071869. PMC 11012492. PMID 38610634.
- ^ Sayer AA (November 2014). "Sarcopenia the new geriatric giant: time to translate research findings into clinical practice". Age and Ageing. 43 (6): 736–737. doi:10.1093/ageing/afu118. PMID 25227204.
- ^ Abate M, Di Iorio A, Di Renzo D, Paganelli R, Saggini R, Abate G (September 2007). "Frailty in the elderly: the physical dimension". Europa Medicophysica. 43 (3): 407–415. PMID 17117147.
- ^ Yarasheski KE (October 2003). "Exercise, aging, and muscle protein metabolism". The Journals of Gerontology. Series A, Biological Sciences and Medical Sciences (Review). 58 (10): M918–M922. doi:10.1093/gerona/58.10.m918. PMID 14570859.
- ^ Liu CJ, Latham NK (July 2009). "Progressive resistance strength training for improving physical function in older adults". The Cochrane Database of Systematic Reviews. 2009 (3): CD002759. doi:10.1002/14651858.cd002759.pub2. PMC 4324332. PMID 19588334.
- ^ Valenzuela PL, Castillo-García A, Morales JS, Izquierdo M, Serra-Rexach JA, Santos-Lozano A, et al. (September 2019). Terjung R (ed.). "Physical Exercise in the Oldest Old". Comprehensive Physiology. 9 (4) (1st ed.). Wiley: 1281–1304. doi:10.1002/cphy.c190002. ISBN 978-0-470-65071-4. PMID 31688965.
- ^ Fragala MS, Cadore EL, Dorgo S, Izquierdo M, Kraemer WJ, Peterson MD, et al. (August 2019). "Resistance Training for Older Adults: Position Statement From the National Strength and Conditioning Association". Journal of Strength and Conditioning Research. 33 (8): 2019–2052. doi:10.1519/JSC.0000000000003230. PMID 31343601.
- ^
 This article incorporates text available under the CC BY 4.0 license. Betts JG, Desaix P, Johnson E, Johnson JE, Korol O, Kruse D, et al. (8 June 2023). Anatomy & Physiology. Houston: OpenStax CNX. 10.6 Exercise and muscle performance. ISBN 978-1-947172-04-3.
This article incorporates text available under the CC BY 4.0 license. Betts JG, Desaix P, Johnson E, Johnson JE, Korol O, Kruse D, et al. (8 June 2023). Anatomy & Physiology. Houston: OpenStax CNX. 10.6 Exercise and muscle performance. ISBN 978-1-947172-04-3.
- ^ a b c Phillips SM (July 2015). "Nutritional supplements in support of resistance exercise to counter age-related sarcopenia". Advances in Nutrition. 6 (4): 452–460. doi:10.3945/an.115.008367. PMC 4496741. PMID 26178029.
- ^ a b c d Sakuma K, Yamaguchi A (28 May 2012). "Sarcopenia and age-related endocrine function". International Journal of Endocrinology. 2012: 127362. doi:10.1155/2012/127362. PMC 3368374. PMID 22690213.
- ^ a b Wakabayashi H, Sakuma K (May 2014). "Comprehensive approach to sarcopenia treatment". Current Clinical Pharmacology. 9 (2): 171–180. doi:10.2174/1574884708666131111192845. PMID 24219006.
- ^ Finkle WD, Greenland S, Ridgeway GK, Adams JL, Frasco MA, Cook MB, et al. (29 January 2014). "Increased risk of non-fatal myocardial infarction following testosterone therapy prescription in men". PLOS ONE. 9 (1): e85805. Bibcode:2014PLoSO...985805F. doi:10.1371/journal.pone.0085805. PMC 3905977. PMID 24489673.
- ^ Vigen R, O'Donnell CI, Barón AE, Grunwald GK, Maddox TM, Bradley SM, et al. (November 2013). "Association of testosterone therapy with mortality, myocardial infarction, and stroke in men with low testosterone levels". JAMA. 310 (17): 1829–1836. doi:10.1001/jama.2013.280386. PMID 24193080.
- ^ Basaria S, Coviello AD, Travison TG, Storer TW, Farwell WR, Jette AM, et al. (July 2010). "Adverse events associated with testosterone administration". The New England Journal of Medicine. 363 (2): 109–122. doi:10.1056/NEJMoa1000485. PMC 3440621. PMID 20592293.
- ^ Robinson SM, Reginster JY, Rizzoli R, Shaw SC, Kanis JA, Bautmans I, et al. (August 2018). "Does nutrition play a role in the prevention and management of sarcopenia?". Clinical Nutrition. 37 (4): 1121–1132. doi:10.1016/j.clnu.2017.08.016. PMC 5796643. PMID 28927897.
- ^ Bauer J, Biolo G, Cederholm T, Cesari M, Cruz-Jentoft AJ, Morley JE, et al. (August 2013). "Evidence-based recommendations for optimal dietary protein intake in older people: a position paper from the PROT-AGE Study Group". Journal of the American Medical Directors Association. 14 (8): 542–559. doi:10.1016/j.jamda.2013.05.021. PMID 23867520.
- ^ Deutz NE, Bauer JM, Barazzoni R, Biolo G, Boirie Y, Bosy-Westphal A, et al. (December 2014). "Protein intake and exercise for optimal muscle function with aging: recommendations from the ESPEN Expert Group". Clinical Nutrition. 33 (6): 929–936. doi:10.1016/j.clnu.2014.04.007. PMC 4208946. PMID 24814383.
- ^ Tessier AJ, Chevalier S (August 2018). "An Update on Protein, Leucine, Omega-3 Fatty Acids, and Vitamin D in the Prevention and Treatment of Sarcopenia and Functional Decline". Nutrients. 10 (8): 1099. doi:10.3390/nu10081099. PMC 6116139. PMID 30115829.
- ^ Fujita S, Volpi E (January 2006). "Amino acids and muscle loss with aging". The Journal of Nutrition. 136 (1 Suppl): 277S–280S. doi:10.1093/jn/136.1.277S. PMC 3183816. PMID 16365098.
- ^ Brioche T, Pagano AF, Py G, Chopard A (August 2016). "Muscle wasting and aging: Experimental models, fatty infiltrations, and prevention" (PDF). Molecular Aspects of Medicine. 50: 56–87. doi:10.1016/j.mam.2016.04.006. PMID 27106402. S2CID 29717535.
- ^ a b Wu H, Xia Y, Jiang J, Du H, Guo X, Liu X, et al. (September 2015). "Effect of beta-hydroxy-beta-methylbutyrate supplementation on muscle loss in older adults: a systematic review and meta-analysis". Archives of Gerontology and Geriatrics. 61 (2): 168–175. doi:10.1016/j.archger.2015.06.020. PMID 26169182.
- ^ Holeček M (August 2017). "Beta-hydroxy-beta-methylbutyrate supplementation and skeletal muscle in healthy and muscle-wasting conditions". Journal of Cachexia, Sarcopenia and Muscle. 8 (4): 529–541. doi:10.1002/jcsm.12208. PMC 5566641. PMID 28493406.
- ^ Xia L, Zhao R, Wan Q, Wu Y, Zhou Y, Wang Y, et al. (November 2020). "Sarcopenia and adverse health-related outcomes: An umbrella review of meta-analyses of observational studies". Cancer Medicine. 9 (21): 7964–7978. doi:10.1002/cam4.3428. PMC 7643685. PMID 32924316.
- ^ Rodrigues F, Domingos C, Monteiro D, Morouço P (January 2022). "A Review on Aging, Sarcopenia, Falls, and Resistance Training in Community-Dwelling Older Adults". International Journal of Environmental Research and Public Health. 19 (2): 874. doi:10.3390/ijerph19020874. PMC 8775372. PMID 35055695.
- ^ Sayer AA, Robinson SM, Patel HP, Shavlakadze T, Cooper C, Grounds MD (March 2013). "New horizons in the pathogenesis, diagnosis and management of sarcopenia". Age and Ageing. 42 (2): 145–150. doi:10.1093/ageing/afs191. PMC 3575121. PMID 23315797.
- ^ Rolland Y, Dray C, Vellas B, Barreto PS (December 2023). "Current and investigational medications for the treatment of sarcopenia". Metabolism. 149: 155597. doi:10.1016/j.metabol.2023.155597. PMID 37348598. S2CID 259232987.
- ^ Fonseca GW, Dworatzek E, Ebner N, Von Haehling S (August 2020). "Selective androgen receptor modulators (SARMs) as pharmacological treatment for muscle wasting in ongoing clinical trials". Expert Opinion on Investigational Drugs. 29 (8): 881–891. doi:10.1080/13543784.2020.1777275. PMID 32476495. S2CID 219174372.
- ^ Christiansen AR, Lipshultz LI, Hotaling JM, Pastuszak AW (March 2020). "Selective androgen receptor modulators: the future of androgen therapy?". Translational Andrology and Urology. 9 (Suppl 2): S135–S148. doi:10.21037/tau.2019.11.02. PMC 7108998. PMID 32257854.
Further reading
[edit]- Fujita S, Volpi E (January 2006). "Amino acids and muscle loss with aging". The Journal of Nutrition (Review). 136 (1 Suppl): 277S–280S. doi:10.1093/jn/136.1.277S. PMC 3183816. PMID 16365098.
- Roubenoff R (December 2007). "Physical activity, inflammation, and muscle loss". Nutrition Reviews. 65 (12 Pt 2): S208–S212. doi:10.1111/j.1753-4887.2007.tb00364.x. PMID 18240550.
- Sharlo K, Tyganov SA, Tomilovskaya E, Popov DV, Saveko AA, Shenkman BS (December 2021). "Effects of Various Muscle Disuse States and Countermeasures on Muscle Molecular Signaling". International Journal of Molecular Sciences. 23 (1): 468. doi:10.3390/ijms23010468. PMC 8745071. PMID 35008893.
