Alcohol and health: Difference between revisions
| Line 428: | Line 428: | ||
==Long-term effects of alcohol== |
==Long-term effects of alcohol== |
||
{{See also|Long-term effects of alcohol}} |
{{See also|Long-term effects of alcohol}} |
||
{{Infobox disease |
|||
|Name = Long-term effects of alcohol |
|||
|Image = |
|||
|Caption = |
|||
|ICD10 = {{ICD10|F|10||f|10}}.1 |
|||
}} |
|||
[[File:Alcohol use disorders world map - DALY - WHO2004.svg|thumb|[[Disability-adjusted life year]] for alcohol use disorders per 100,000 inhabitants in 2004.<div class="references-small" style="-moz-column-count:3; column-count:3;"> |
|||
{{legend|#b3b3b3|no data}} |
|||
{{legend|#ffff65|less than 50}} |
|||
{{legend|#fff200|50–150}} |
|||
{{legend|#ffdc00|150–250}} |
|||
{{legend|#ffc600|250–350}} |
|||
{{legend|#ffb000|350–450}} |
|||
{{legend|#ff9a00|450–550}} |
|||
{{legend|#ff8400|550–650}} |
|||
{{legend|#ff6e00|650–750}} |
|||
{{legend|#ff5800|750–850}} |
|||
{{legend|#ff4200|850–950}} |
|||
{{legend|#ff2c00|950–1050}} |
|||
{{legend|#cb0000|more than 1050}} |
|||
</div>]] |
|||
[[File:Alcohol by Country.png|thumb|200px|Total recorded alcohol per capita consumption (15+), in litres of pure alcohol<ref>[http://www.who.int/entity/substance_abuse/publications/global_status_report_2004_overview.pdf Global Status Report on Alcohol 2004]</ref>]] |
|||
[[File:Possible long-term effects of ethanol.svg|thumb|300px|right|Most significant of the possible long-term effects of ethanol. Consumption of alcohol by pregnant mothers may result in [[fetal alcohol syndrome]].]] |
|||
'''The long term effects of alcohol''' ([[ethanol]]) consumption range from [[Alcohol and cardiovascular disease|cardioprotective health benefits]] for low to moderate alcohol consumption in industrialized societies with higher rates of cardiovascular disease<ref>Association of alcohol consumption with selected cardiovascular disease outcomes: a systematic review and meta-analysis. |
|||
Paul E Ronksley, Susan E Brien, Barbara J Turner, Kenneth J Mukamal, William A Ghali |
|||
BMJ 2011;342:d671</ref><ref>Prospective study of alcohol drinking patterns and coronary heart disease in women and men. Janne Tolstrup, Majken K Jensen, Tjønneland Anne, Kim Overvad, Kenneth J Mukamal, and Morten Grønbæk. |
|||
BMJ 2006;332:1244.</ref> to severe detrimental effects in cases of chronic [[alcohol abuse]].<ref>No authors listed (2000). "Health Risks and Benefits of Alcohol Consumption Health Risks and Benefits of Alcohol Consumption". Alcohol Res Health 24 (1): 5–11.</ref> High levels of alcohol consumption are associated with an increased risk of [[alcoholism]], [[malnutrition]], [[chronic pancreatitis]], [[alcoholic liver disease]], and [[cancer]]. In addition damage to the [[central nervous system]] and [[peripheral nervous system]] can occur from chronic alcohol abuse.<ref>{{cite journal|author=Müller D, Koch RD, von Specht H, Völker W, Münch EM|title=[Neurophysiologic findings in chronic alcohol abuse]|language=German|journal=Psychiatr Neurol Med Psychol (Leipz)|volume=37|issue=3|pages=129–32|year=1985|month=March|pmid=2988001}}</ref><ref>{{cite journal|author=Testino G|title=Alcoholic diseases in hepato-gastroenterology: a point of view|journal=Hepatogastroenterology|volume=55|issue=82-83|pages=371–7|year=2008|pmid=18613369}}</ref> Long-term use of alcohol in excessive quantities is capable of damaging nearly every organ and system in the body.<ref>{{cite book|editor1-first=Woody|editor1-last=Caan|editor2-first=Jackie de|editor2-last=Belleroche|title=Drink, Drugs and Dependence: From Science to Clinical Practice|url=http://books.google.com/?id=nPvbDUw4w5QC|edition=1st|date=11 April 2002|publisher=Routledge|isbn=978-0-415-27891-1|pages=19–20}}</ref> The developing adolescent brain is particularly vulnerable to the toxic effects of alcohol.{{citation needed|date=January 2013}} In addition, the developing fetal brain is also vulnerable, and [[fetal alcohol syndrome]] (FAS) may result if pregnant mothers consume alcohol.<ref>{{Cite journal|last1=Mellon|first1=RD.|last2=Simone|first2=AF.|last3=Rappaport|first3=BA.|title=Use of anesthetic agents in neonates and young children|url=http://www.anesthesia-analgesia.org/cgi/content/full/104/3/509|journal=Anesth Analg|volume=104|issue=3|pages=509–20|month=Mar|year=2007|doi=10.1213/01.ane.0000255729.96438.b0|pmid=17312200}}</ref> |
|||
The inverse relation in Western cultures between alcohol consumption and cardiovascular disease has been known for over 100 years.<ref>{{cite journal |author=Cabot, R.C. |title=The relation of alcohol to arterioscleroisis |journal=Journal of the American Medical Association |year=1904 |volume=43 |pages=774–775}}</ref> There has been reluctance by many physicians, however, to promote alcohol consumption given the many concerns associated with chronic alcohol abuse. Some even suggest that alcohol should be regarded as a recreational drug, and prefer exercise and good nutrition to combat cardiovascular disease.<ref name="Sellman-2009">{{Cite journal|last1=Sellman|first1=D.|last2=Connor|first2=J.|last3=Robinson|first3=G.|last4=Jackson|first4=R.|title=Alcohol cardio-protection has been talked up.|journal=N Z Med J|volume=122|issue=1303|pages=97–101|year=2009|pmid=19851424}}</ref><ref>{{Cite journal|last1=Sinkiewicz|first1=W.|last2=Weglarz|first2=M.|title=[Alcohol and wine and cardiovascular diseases in epidemiologic studies]|journal=Przegl Lek|volume=66|issue=5|pages=233–8|year=2009|pmid=19739580}}</ref> Others have argued that the benefits of moderate alcohol consumption may be outweighed by other increased risks, including those of [[injuries]], [[violence]], [[fetal]] damage, [[liver disease]], and certain forms of [[cancer]].<ref name="Andréasson-"/> |
|||
===Scientific Studies=== |
|||
====Background==== |
|||
The adverse effects of long-term excessive use of alcohol are close to those seen with other sedative-hypnotics (apart from organ toxicity which is much more problematic with alcohol). [[Withdrawal]] effects and dependence are also almost identical.<ref>{{cite book|last1=Gitlow|first1=Stuart|title=Substance Use Disorders: A Practical Guide|url=http://books.google.com/?id=rbrSdWVerBUC|edition=2nd|date=1 October 2006|publisher=Lippincott Williams and Wilkins|location=USA|isbn=978-0-7817-6998-3|pages=101–103}}</ref> Alcohol at moderate levels has some positive and negative effects on health. The negative effects include increased risk of [[liver diseases]], [[oropharyngeal]] [[cancer]], [[esophageal cancer]] and [[pancreatitis]]. Conversely moderate intake of alcohol may have some beneficial effects on [[gastritis]] and [[cholelithiasis]].<ref>{{cite journal|author=Taylor B, Rehm J, Gmel G|title=Moderate alcohol consumption and the gastrointestinal tract|journal=Dig Dis|volume=23|issue=3-4|pages=170–6|year=2005|pmid=16508280|doi=10.1159/000090163|url=http://content.karger.com/produktedb/produkte.asp?typ=fulltext&file=DDI20050233_4170}}</ref> Chronic alcohol misuse and abuse has serious effects on physical and mental health. Chronic excess alcohol intake, or alcohol dependence, can lead to a wide range of [[neuropsychiatric]] or [[neurological]] impairment, [[cardiovascular]] disease, [[liver disease]], and [[malignant neoplasms]]. The psychiatric disorders which are associated with alcoholism include [[major depression]], [[dysthymia]], [[mania]], [[hypomania]], [[panic disorder]], [[phobias]], [[generalized anxiety disorder]], [[personality disorders]], [[schizophrenia]], [[suicide]], [[neurologic]] deficits (e.g. impairments of [[working memory]], [[emotions]], [[executive functions]], [[visuospatial]] abilities and [[gait]] and [[balance (ability)|balance]]) and [[brain damage]]. Alcohol dependence is associated with [[hypertension]], [[coronary heart disease]], and [[ischemic stroke]], [[cancer]] of the [[respiratory system]], and also [[cancers]] of the [[digestive system]], [[liver]], [[breast]] and [[ovaries]]. Heavy drinking is associated with [[liver disease]], such as [[cirrhosis]].<ref>{{cite journal|author=Cargiulo T|title=Understanding the health impact of alcohol dependence|journal=Am J Health Syst Pharm|volume=64|issue=5 Suppl 3|pages=S5–11|year=2007|month=March|pmid=17322182|doi=10.2146/ajhp060647|url=}}</ref> Excessive alcohol consumption can have a negative [[Impact of alcohol on aging|impact on aging]].<ref name="pmid16350768">{{cite journal|author=Stevenson JS|title=Alcohol use, misuse, abuse, and dependence in later adulthood|journal=Annu Rev Nurs Res|volume=23|pages=245–80|year=2005|pmid=16350768}}</ref> |
|||
Recent studies have focused on understanding the mechanisms by which moderate alcohol consumption confers cardiovascular benefit.<ref>{{cite journal|author=Vliegenthart R, Oei HH, van den Elzen AP, ''et al.''|title=Alcohol consumption and coronary calcification in a general population|journal=Arch. Intern. Med.|volume=164|issue=21|pages=2355–60|year=2004|month=November|pmid=15557415|doi=10.1001/archinte.164.21.2355}}<br /> |
|||
{{cite journal|author=Koppes LL, Twisk JW, Snel J, Van Mechelen W, Kemper HC|title=Blood cholesterol levels of 32-year-old alcohol consumers are better than of nonconsumers|journal=Pharmacol Biochem Behav.|volume=66|issue=1|pages=163–7|year=2000|month=May|pmid=10837856|url=http://linkinghub.elsevier.com/retrieve/pii/S0091-3057(00)00195-7|doi=10.1016/S0091-3057(00)00195-7}}<br /> |
|||
{{cite journal|author=Albert MA, Glynn RJ, Ridker PM|title=Alcohol consumption and plasma concentration of C-reactive protein|journal=Circulation|volume=107|issue=3|pages=443–7|year=2003|month=January|pmid=12551869|url=http://circ.ahajournals.org/cgi/pmidlookup?view=long&pmid=12551869|doi=10.1161/01.CIR.0000045669.16499.EC}}<br /> |
|||
{{cite journal|author=Baer DJ, Judd JT, Clevidence BA, ''et al.''|title=Moderate alcohol consumption lowers risk factors for cardiovascular disease in postmenopausal women fed a controlled diet|journal=Am J Clin Nutr.|volume=75|issue=3|pages=593–9|date=1 March 2002|pmid=11864868|url=http://www.ajcn.org/cgi/pmidlookup?view=long&pmid=11864868}}</ref> One study has suggested a beneficial effect of alcohol on patients with hypertension.<ref>{{cite journal|author=Catena C, Novello M, Dotto L, De Marchi S, Sechi LA|title=Serum lipoprotein(a) concentrations and alcohol consumption in hypertension: possible relevance for cardiovascular damage|journal=J. Hypertens.|volume=21|issue=2|pages=281–8|year=2003|month=February|pmid=12569257|doi=10.1097/01.hjh.0000052436.12292.26}}</ref> |
|||
====Maximum quantity recommended==== |
|||
{{Further|Recommended maximum intake of alcoholic beverages}} |
|||
Different countries recommend different maximum quantities. For most countries, the maximum quantity for men is 140 g–210 g per week. For women, the range is 84 g–140 g per week.{{citation needed|date=January 2013}} Most countries recommend total abstinence whilst pregnant or breastfeeding. |
|||
===Alcohol-related deaths=== |
|||
Over-consumption of alcohol is one of the leading [[List of preventable causes of death|preventable causes of death]] worldwide.<ref>{{cite journal|author=Lopez AD, Mathers CD, Ezzati M, Jamison DT, Murray CJ|title=Global and regional burden of disease and risk factors, 2001: systematic analysis of population health data|journal=Lancet|volume=367|issue=9524|pages=1747–57|year=2006|month=May|pmid=16731270|doi=10.1016/S0140-6736(06)68770-9|url=}}</ref> One study links alcohol to 1 in every 25 deaths worldwide and that 5% of years lived with disability are attributable to alcohol consumption.<ref>BBC [http://news.bbc.co.uk/1/hi/health/8118475.stm Alcohol link to one in 25 deaths]</ref><ref>Jürgen Rehm, Colin Mathers, Svetlana Popova, Montarat Thavorncharoensap, Yot Teerawattananon, Jayadeep Patra [http://www.thelancet.com/journals/lancet/article/PIIS0140-6736(09)60746-7/abstract Global burden of disease and injury and economic cost attributable to alcohol use and alcohol-use disorders] ''The Lancet'', Volume 373, Issue 9682, Pages 2223 - 2233, 27 June 2009 {{doi|10.1016/S0140-6736(09)60746-7}}</ref> |
|||
Countries collect statistics on alcohol-related deaths. While some categories relate to short-term effects, such as accidents, many relate to long-term effects of alcohol. |
|||
<!-- Countries are in alphabetical order --> |
|||
====Russia==== |
|||
{{Main|Alcoholism in Russia}} |
|||
One study claims that "excessive alcohol consumption in Russia, particularly by men, has in recent years caused more than half of all the deaths at ages 15-54 years."<ref>IARC [http://www.iarc.fr/en/media-centre/iarcnews/2009/IARCLancet270709.pdf Alcohol causes more than half of all the premature deaths in Russian adults]</ref> However, there are some difficulties with this study. For instance the same study also found a protective effect of heavy drinking on breast cancer mortality. This contradicts the well established scientific view that alcohol increases breast cancer risk.<ref name="Tjønneland-2007">{{Cite journal|last1=Tjønneland|first1=A.|last2=Christensen|first2=J.|last3=Olsen|first3=A.|last4=Stripp|first4=C.|last5=Thomsen|first5=BL.|last6=Overvad|first6=K.|last7=Peeters|first7=PH.|last8=van Gils|first8=CH.|last9=Bueno-de-Mesquita|first9=HB.|title=Alcohol intake and breast cancer risk: the European Prospective Investigation into Cancer and Nutrition (EPIC)|journal=Cancer Causes Control|volume=18|issue=4|pages=361–73|month=May|year=2007|doi=10.1007/s10552-006-0112-9|PMID=17364225}}</ref> On this account in further correspondence it was advised that "careful interpretation of mortality statistics in relation to alcohol use is needed, taking into account other relevant risk factors, incidence, and survival."<ref name="Soerjomataram-2009">{{Cite journal|last1=Soerjomataram|first1=I.|last2=de Vries|first2=E.|last3=Coebergh|first3=JW.|title=Did alcohol protect against death from breast cancer in Russia?|journal=Lancet|volume=374|issue=9694|pages=975; author reply 975–6|month=Sep|year=2009|doi=10.1016/S0140-6736(09)61657-3|PMID=19766875}}</ref> |
|||
The authors replied that "whether or not the apparent shortfall in breast cancer mortality among heavy drinkers is real, it accounts for only about 0·1% of adult deaths in Russia. Careful interpretation of it is therefore of little relevance to the findings for alcohol and overall mortality". |
|||
====United Kingdom==== |
|||
Alcohol-related deaths in the United Kingdom are coded using the Tenth Revision of the [[ICD|International Classification of Diseases]] (ICD-10).<ref name=NSO>[http://www.statistics.gov.uk/statbase/Product.asp?vlnk=14496 Alcohol-related deaths in the United Kingdom] and links therefrom</ref> |
|||
[[ICD-10]] comprises: |
|||
* Mental and behavioural disorders due to use of alcohol – ICD-10 F10 |
|||
* Degeneration of nervous system due to alcohol – ICD-10 G31.2 |
|||
* Alcoholic polyneuropathy – ICD-10 G62.1 |
|||
* Alcoholic cardiomyopathy – ICD-10 I42.6 |
|||
* Alcoholic gastritis – ICD-10 K29.2 |
|||
* Alcoholic liver disease – ICD-10 K70 |
|||
* Chronic hepatitis, not elsewhere classified – ICD-10 K73 |
|||
* Fibrosis and cirrhosis of liver – ICD-10 K74 (Excluding K74.3-K74.5 – Biliary cirrhosis) |
|||
* Alcohol induced chronic pancreatitis – ICD-10 K86.0 |
|||
* Accidental poisoning by and exposure to alcohol – ICD-10 X45 |
|||
* Intentional self-poisoning by and exposure to alcohol – ICD-10 X65 |
|||
* Poisoning by and exposure to alcohol, undetermined intent – ICD-10 Y15 |
|||
UK statistical bodies report that "There were 8,724 alcohol-related deaths in 2007, lower than 2006, but more than double the 4,144 recorded in 1991. The alcohol-related death rate was 13.3 per 100,000 population in 2007, compared with 6.9 per 100,000 population in 1991."<ref>[http://www.statistics.gov.uk/cci/nugget.asp?id=1091 Alcohol Deaths: Rates stabilise in the UK]</ref> |
|||
In Scotland, the NHS estimate that in 2003 one in every 20 deaths could be attributed to alcohol.<ref>BBC [http://news.bbc.co.uk/1/hi/scotland/8126129.stm Alcohol 'kills one in 20 Scots'] 30 June 2009</ref> |
|||
A 2009 study found that 9,000 people are dying from alcohol-related diseases every year, three times the number 25 years previously.<ref>Sam Lister [http://www.timesonline.co.uk/tol/life_and_style/health/article6880210.ece The price of alcohol: an extra 6,000 early deaths a year] ''The Times'', 19 October 2009</ref> |
|||
====United States==== |
|||
The [[Centers for Disease Control and Prevention]] report, "From 2001–2005, there were approximately 79,000 deaths annually attributable to excessive alcohol use. In fact, excessive alcohol use is the 3rd leading lifestyle-related cause of death for people in the United States each year."<ref>Centers for Disease Control and Prevention [http://www.cdc.gov/alcohol/ Alcohol and Public Health]</ref> A 1993 study estimated US deaths through alcohol at 100,000.<ref>{{cite journal|doi=10.1001/jama.270.18.2207|last1=McGinnis|first1=J. Michael|last2=Foege|first2=William H.|author-separator =,|year=1993|title=Actual Causes of Death in the United States|url=http://jama.ama-assn.org/cgi/reprint/270/18/2207?ijkey=f6b2a35ebda67d08b66074771b6a6000007c3770|journal=JAMA|volume=270|issue=18|pages=2207–2212|pmid=8411605}}</ref> |
|||
====Overall mortality==== |
|||
Extensive research of Western cultures has consistently shown increased survival associated with light to moderate alcohol consumption.<ref>Di Castelnuovo A, Costanzo S, Bagnardi V, Donati MB, Iacoviello L, de Gaetano G. Alcohol dosing and total mortality in men and women: an updated meta-analysis of 34 prospective studies. Arch Intern Med. 2006 Dec 11-25;166(22):2437-45.</ref> A 23-year [[prospective study]] of 12,000 male [[United Kingdom|British]] [[physician]]s aged 48–78, found that overall mortality was significantly lower in current drinkers compared to non-drinkers even after correction for ex-drinkers. This benefit was strongest for ischemic heart disease, but was also noted for other vascular disease and respiratory disease. Death rate amongst current drinkers was higher for 'alcohol augmentable' disease such as liver disease and oral cancers, but these deaths were much less common than cardiovascular and respiratory deaths. The lowest mortality rate was found for consumption of 8 to 14 'units' per week. In the UK a unit is defined as 10ml or 8g of pure alcohol.<ref>http://www.drinkaware.co.uk/facts/frequently-asked-questions#what_is_unit</ref> Higher consumption increased overall mortality rate, but not above that of non-drinkers.<ref name="Doll R, Peto R, Boreham J, Sutherland I 2005 199–204">{{cite journal|author=Doll R, Peto R, Boreham J, Sutherland I|title=Mortality in relation to alcohol consumption: a prospective study among male British doctors|journal=Int J Epidemiol|volume=34|issue=1|pages=199–204|year=2005|month=February|pmid=15647313|doi=10.1093/ije/dyh369|url=http://ije.oxfordjournals.org/cgi/content/full/34/1/199}}</ref> |
|||
This is consistent with other research that found a J-curve dependency between alcohol consumption and total mortality among middle aged and older men. While the mortality rates of ex-drinkers and heavy drinkers are significantly elevated, the all-cause mortality rates may be 15-18% lower among moderate drinkers. Although the definition of a [[alcohol equivalence|drink]] varies between studies and countries, this meta-analysis found that low levels of alcohol intake, defined as 1-2 drinks per day for women and 2-4 drinks per day for men, was associated with lower mortality than abstainers.<ref name="Di Castelnuovo-">{{Cite journal|last1=Di Castelnuovo|first1=A.|last2=Costanzo|first2=S.|last3=Bagnardi|first3=V.|last4=Donati|first4=MB.|last5=Iacoviello|first5=L.|last6=de Gaetano|first6=G.|title=Alcohol dosing and total mortality in men and women: an updated meta-analysis of 34 prospective studies.|journal=Arch Intern Med|volume=166|issue=22|pages=2437–45|doi=10.1001/archinte.166.22.2437|PMID=17159008}}</ref> This claim was challenged by another study<ref name="Fillmore-2007">{{Cite journal|last1=Fillmore|first1=KM.|last2=Stockwell|first2=T.|last3=Chikritzhs|first3=T.|last4=Bostrom|first4=A.|last5=Kerr|first5=W.|title=Moderate alcohol use and reduced mortality risk: systematic error in prospective studies and new hypotheses|journal=Ann Epidemiol|volume=17|issue=5 Suppl|pages=S16-23|month=May|year=2007|doi=10.1016/j.annepidem.2007.01.005|PMID=17478320}}</ref><ref name="Chikritzhs-2009">{{Cite journal|last1=Chikritzhs|first1=T.|last2=Fillmore|first2=K.|last3=Stockwell|first3=T.|title=A healthy dose of scepticism: four good reasons to think again about protective effects of alcohol on coronary heart disease|journal=Drug Alcohol Rev|volume=28|issue=4|pages=441–4|month=Jul|year=2009|doi=10.1111/j.1465-3362.2009.00052.x|PMID=19594799}}</ref> that found that in certain low quality studies occasional drinkers or ex-drinkers were included as abstainers, resulting in the increased mortality in that group. However, the J-curve for total and CHD mortality was reconfirmed by studies that took the mentioned confounders into account.<ref name="Ann Epidemiol 2007">Ann Epidemiol. 2007. Volume 17, Issue 5. Alcohol Drinking and Total Mortality Risk Arthur L. Klatsky, MD, Natalia Udaltsova, PhD</ref><ref name="Lee-2009">{{Cite journal|last1=Lee|first1=SJ.|last2=Sudore|first2=RL.|last3=Williams|first3=BA.|last4=Lindquist|first4=K.|last5=Chen|first5=HL.|last6=Covinsky|first6=KE.|title=Functional limitations, socioeconomic status, and all-cause mortality in moderate alcohol drinkers|journal=J Am Geriatr Soc|volume=57|issue=6|pages=955–62|month=Jun|year=2009|doi=10.1111/j.1532-5415.2009.02184.x|PMID=19473456}}</ref><ref name="Arriola-2010">{{Cite journal|last1=Arriola|first1=L.|last2=Martinez-Camblor|first2=P.|last3=Larrañaga|first3=N.|last4=Basterretxea|first4=M.|last5=Amiano|first5=P.|last6=Moreno-Iribas|first6=C.|last7=Carracedo|first7=R.|last8=Agudo|first8=A.|last9=Ardanaz|first9=E.|title=Alcohol intake and the risk of coronary heart disease in the Spanish EPIC cohort study|journal=Heart|volume=96|issue=2|pages=124–30|month=Jan|year=2010|doi=10.1136/hrt.2009.173419|PMID=19933099}}</ref><ref name="Holahan-2010">{{Cite journal|last1=Holahan|first1=CJ.|last2=Schutte|first2=KK.|last3=Brennan|first3=PL.|last4=Holahan|first4=CK.|last5=Moos|first5=BS.|last6=Moos|first6=RH.|title=Late-life alcohol consumption and 20-year mortality.|journal=Alcohol Clin Exp Res|volume=34|issue=11|pages=1961–71|month=Nov|year=2010|doi=10.1111/j.1530-0277.2010.01286.x|PMID=20735372}}</ref> |
|||
It has been suggested that the observed decrease in mortality of light-to-moderate drinkers compared to never drinkers might be partially explained by superior health and social status of the drinking group;<ref name="Hansel-2010">{{Cite journal|last1=Hansel|first1=B.|last2=Thomas|first2=F.|last3=Pannier|first3=B.|last4=Bean|first4=K.|last5=Kontush|first5=A.|last6=Chapman|first6=MJ.|last7=Guize|first7=L.|last8=Bruckert|first8=E.|title=Relationship between alcohol intake, health and social status and cardiovascular risk factors in the urban Paris-Ile-De-France Cohort: is the cardioprotective action of alcohol a myth?|journal=Eur J Clin Nutr|volume=64|issue=6|pages=561–8|month=Jun|year=2010|doi=10.1038/ejcn.2010.61|PMID=20485310}}</ref> however, the protective effect of alcohol in light to moderate drinkers remains significant even after adjusting for these confounders.<ref name="Lee-2009"/><ref name="Holahan-2010"/> Additionally, confounders such as underreporting of alcohol intake might lead to the underestimation of how much mortality is reduced in light-to-moderate drinkers.<ref name="Ann Epidemiol 2007"/><ref name="Klatsky-2008">{{Cite journal|last1=Klatsky|first1=AL.|title=Invited commentary: never, or hardly ever? It could make a difference.|journal=Am J Epidemiol|volume=168|issue=8|pages=872–5; discussion 876–7|month=Oct|year=2008|doi=10.1093/aje/kwn192|PMID=18701441}}</ref> |
|||
A 2010 study confirmed the beneficial effect of moderate alcohol consumption on mortality.<ref name="Holahan-2010"/> Subjects were grouped into abstainers, light, moderate, and heavy drinkers. The order of mortality rates from lowest to highest were moderate, light, heavy, and abstainers. The increased risk for abstainers was twice the mortality rate as for moderate drinkers. This study specifically sought to control for confounding factors including the problem of ex-drinkers considered as non-drinkers.<ref name="Holahan-2010"/> According to another study, drinkers with heavy drinking occasions (six or more drinks at a time) have a 57% higher all-cause mortality than drinkers without heavy drinking occasions.<ref name="Laatikainen-2003">{{Cite journal|last1=Laatikainen|first1=T.|last2=Manninen|first2=L.|last3=Poikolainen|first3=K.|last4=Vartiainen|first4=E.|title=Increased mortality related to heavy alcohol intake pattern.|journal=J Epidemiol Community Health|volume=57|issue=5|pages=379–84|month=May|year=2003|PMID=12700224|pmc=1732462}}</ref> |
|||
In contrast to studies of Western cultures, research in other cultures has yielded some opposite findings. The landmark INTERHEART Study has revealed that alcohol consumption in South Asians was not protective against CAD in sharp contrast to other populations who benefit from it.<ref name="Risk Factors">{{cite journal|coauthors=Joshi, Prashant; Islam, Shofiqul; Pais, Prem; Reddy, Srinath; Dorairaj, Prabhakaran; Kazmi, Khawar; Pandey, Mrigendra Raj; Haque, Sirajul; Mendis, Shanthi; Rangarajan, Sumathy; Yusuf, Salim|title=Risk Factors for Early Myocardial Infarction in South Asians Compared With Individuals in Other Countries|journal=JAMA|date=17|year=2007|month=January|volume=297|issue=3|pages=286–294|url=http://jama.ama-assn.org/content/297/3/286.full.pdf|accessdate=20 March 2012|publisher=American Medical Association}}</ref> In fact Asian Indians who consume alcohol had a 60% higher risk of heart attack which was greater with local spirits (80%) than branded spirits (50%).<ref name=Atherosclerosis>{{cite journal|coauthors=Roy A, Prabhakaran D, Jeemon P, Thankappan KR, Mohan V, Ramakrishnan L, Joshi P, Ahmed F, Mohan BV, Saran RK, Sinha N, Reddy KS;|title=Impact of alcohol on coronary heart disease in Indian men.|journal=Atherosclerosis|date=26|year=2010|month=February|volume=210|issue=2|pages=531–535|pmid=20226461|accessdate=20 March 2012|doi=10.1016/j.atherosclerosis.2010.02.033}}</ref> The harm was observed in alcohol users classified as occasional as well as regular light, moderate, and heavy consumers.<ref name=Atherosclerosis /> |
|||
Another large study of 4465 subjects in India also confirmed the possible harm of alcohol consumption on coronary risk in men. Compared to lifetime abstainers, alcohol users had higher blood sugar (2 mg/dl), blood pressure (2 mm Hg) levels, and the HDL-C levels (2 mg/dl) and significantly higher tobacco use (63% vs. 21%).<ref name=Atherosclerosis /> |
|||
===Cardiovascular system=== |
|||
{{main|Alcohol and cardiovascular disease}} |
|||
A meta-analysis of 34 studies found a reduced risk of mortality from coronary heart disease in men who drank 2 - 4 drinks per day and women who drank 1 - 2 drinks per day.<ref name="Di Castelnuovo-">{{Cite journal|last1=Di Castelnuovo|first1=A.|last2=Costanzo|first2=S.|last3=Bagnardi|first3=V.|last4=Donati|first4=MB.|last5=Iacoviello|first5=L.|last6=de Gaetano|first6=G.|title=Alcohol dosing and total mortality in men and women: an updated meta-analysis of 34 prospective studies.|url=http://archinte.ama-assn.org/cgi/content/full/166/22/2437|journal=Arch Intern Med|volume=166|issue=22|pages=2437–45|month=December|year=2006|doi=10.1001/archinte.166.22.2437|pmid=17159008}}</ref> Alcohol has been found to have [[anticoagulant]] properties.<ref name=Mennen>{{cite journal|author=Mennen LI, Balkau B, Vol S, Cacès E, Eschwège E|title=Fibrinogen: a possible link between alcohol consumption and cardiovascular disease? DESIR Study Group|journal=Arterioscler Thromb Vasc Biol.|volume=19|issue=4|pages=887–92|date=1 April 1999|pmid=10195914|url=http://atvb.ahajournals.org/cgi/pmidlookup?view=long&pmid=10195914}}</ref><ref>{{cite journal|author=Paassilta M, Kervinen K, Rantala AO, ''et al.''|title=Social alcohol consumption and low Lp(a) lipoprotein concentrations in middle aged Finnish men: population based study|journal=BMJ|volume=316|issue=7131|pages=594–5|date=14 February 1998|pmid=9518912|pmc=28464|url=http://bmj.com/cgi/pmidlookup?view=long&pmid=9518912}}</ref> [[Thrombosis]] is lower among moderate drinkers than abstainers.<ref>{{cite journal|author=Lacoste L, Hung J, Lam JY|title=Acute and delayed antithrombotic effects of alcohol in humans|journal=Am J Cardiol.|volume=87|issue=1|pages=82–5|year=2001|month=January|pmid=11137839|url=http://linkinghub.elsevier.com/retrieve/pii/S0002-9149(00)01277-7|doi=10.1016/S0002-9149(00)01277-7}}<br />{{cite journal|author=Pahor M, Guralnik JM, Havlik RJ, ''et al.''|title=Alcohol consumption and risk of deep venous thrombosis and pulmonary embolism in older persons|journal=J Am Geriatr Soc|volume=44|issue=9|pages=1030–7|year=1996|month=September|pmid=8790226}}<br />Ridker, P., ''et al.'' Moderate alcohol intake may reduce risk of thrombosis. American Medical Association press release, September 22, 1994<br />{{cite book|author=Ridker, P.|chapter=The Pathogenesis of Atherosclerosis and Acute Thrombosis|editor=Manson, JoAnn E.|title=Prevention of myocardial infarction|publisher=Oxford University Press|location=Oxford [Oxfordshire]|year=1996|isbn=0-19-508582-5}}</ref> A meta-analysis of randomized trials found that alcohol consumption in moderation decreases serum levels of fibrinogen, a protein that promotes clot formation, while it increases levels of tissue type plasminogen activator, an enzyme that helps dissolve clots.<ref>{{Cite journal|last1=Rimm|first1=EB.|last2=Williams|first2=P.|last3=Fosher|first3=K.|last4=Criqui|first4=M.|last5=Stampfer|first5=MJ.|title=Moderate alcohol intake and lower risk of coronary heart disease: meta-analysis of effects on lipids and haemostatic factors.|journal=BMJ|volume=319|issue=7224|pages=1523–8|month=Dec|year=1999|pmid=10591709|pmc=28294}}</ref> These changes were estimated to reduce coronary heart disese risk by about 24%. |
|||
Serum levels of C-reactive protein (CRP), a marker of inflammation and predictor of CHD (coronary heart disease) risk, are lower in moderate drinkers than in those who abstain from alcohol, suggesting that alcohol consumption in moderation might have anti-inflammatory effects.<ref name="Albert-2003">{{Cite journal|last1=Albert|first1=MA.|last2=Glynn|first2=RJ.|last3=Ridker|first3=PM.|title=Alcohol consumption and plasma concentration of C-reactive protein|journal=Circulation|volume=107|issue=3|pages=443–7|month=Jan|year=2003|doi=10.1161/01.CIR.0000045669.16499.EC|pmid=12551869}}</ref><ref name="Stewart-">{{Cite journal|last1=Stewart|first1=SH.|last2=Mainous|first2=AG.|last3=Gilbert|first3=G.|title=Relation between alcohol consumption and C-reactive protein levels in the adult US population|url=http://www.jabfm.org/cgi/reprint/15/6/437.pdf|format=PDF|journal=J Am Board Fam Pract|volume=15|issue=6|pages=437–42|year=2002|pmid=12463288}}</ref><ref name="Imhof-2001">{{Cite journal|last1=Imhof|first1=A.|last2=Froehlich|first2=M.|last3=Brenner|first3=H.|last4=Boeing|first4=H.|last5=Pepys|first5=MB.|last6=Koenig|first6=W.|title=Effect of alcohol consumption on systemic markers of inflammation|journal=Lancet|volume=357|issue=9258|pages=763–7|month=Mar|year=2001|doi=10.1016/S0140-6736(00)04170-2|pmid=11253971}}</ref> |
|||
Despite epidemiological evidence, many have cautioned against recommendations for the use of alcohol for health benefits. A physician from the [[World Health Organisation]] labeled such alcohol promotion as "ridiculous and dangerous".<ref>{{cite journal|author=Abdulla S|title=Is alcohol really good for you?|journal=J R Soc Med|volume=90|issue=12|pages=651|year=1997|month=December|pmid=9496287|pmc=1296731|doi=}}</ref><ref>{{cite journal|author=Naimi TS, Brown DW, Brewer RD, ''et al.''|title=Cardiovascular risk factors and confounders among nondrinking and moderate-drinking U.S. adults|journal=Am J Prev Med|volume=28|issue=4|pages=369–73|year=2005|month=May|pmid=15831343|doi=10.1016/j.amepre.2005.01.011}}</ref> One reviewer has noted, "Despite the wealth of observational data, it is not absolutely clear that alcohol reduces cardiovascular risk, because no randomized controlled trials have been performed. Alcohol should never be recommended to patients to reduce cardiovascular risk as a substitute for the well-proven alternatives of appropriate diet, exercise, and drugs."<ref name="Vogel-2002">{{Cite journal|last1=Vogel|first1=RA.|title=Alcohol, heart disease, and mortality: a review.|journal=Rev Cardiovasc Med|volume=3|issue=1|pages=7–13|year=2002|pmid=12439349}}</ref> It has been argued{{Who|date=June 2011}} that the health benefits from alcohol are at best debatable and may have been exaggerated by the [[alcohol industry]]. Some investigators hold that alcohol should be regarded as a recreational drug with potentially serious adverse effects on health and should not be promoted for cardio-protection.<ref name="Sellman-2009"/> |
|||
Nevertheless, a large prospective non-randomized study has shown that moderate alcohol intake in individuals already at low risk based on body mass index, physical activity, smoking, and diet, yields further improvement in cardiovascular risk.<ref name=Sesso>{{cite journal |author=Sesso HD, Stampfer MJ, Rosner B, Hennekens CH, Manson JE, Gaziano JM |title=Seven-Year Changes in Alcohol Consumption and Subsequent Risk of Cardiovascular Disease in Men |journal=Arch Intern Med |volume=160 |issue=17 |pages=2605–12 |year=2000 |url=http://archinte.ama-assn.org/cgi/content/full/160/17/2605 |doi=10.1001/archinte.160.17.2605 |pmid=10999974}}</ref> |
|||
====Peripheral arterial disease==== |
|||
"Moderate alcohol consumption appears to decrease the risk of PAD in apparently healthy men."<ref>{{cite journal|author=Camargo CA, Stampfer MJ, Glynn RJ, ''et al.''|title=Prospective study of moderate alcohol consumption and risk of peripheral arterial disease in US male physicians|journal=Circulation|volume=95|issue=3|pages=577–80|date=4 February 1997|pmid=9024142|url=http://www.circ.ahajournals.org/cgi/content/full/95/3/577}}</ref> "In this large population-based study, moderatable alcohol consumption was inversely associated with peripheral arterial disease in women but not in men. Residual confounding by smoking may have influenced the results. Among nonsmokers an inverse association was found between alcohol consumption and peripheral arterial disease in both men and women."<ref>{{cite journal|author=Vliegenthart R, Geleijnse JM, Hofman A, ''et al.''|title=Alcohol consumption and risk of peripheral arterial disease: the Rotterdam study|journal=Am J Epidemiol.|volume=155|issue=4|pages=332–8|year=2002|month=February|pmid=11836197|url=http://aje.oxfordjournals.org/cgi/content/full/155/4/332|doi=10.1093/aje/155.4.332}}</ref><ref>{{cite journal|author=Mingardi R, Avogaro A, Noventa F, ''et al.''|title=Alcohol intake is associated with a lower prevalence of peripheral vascular disease in non-insulin dependent diabetic women|journal=Nutrition Metabolism and Cardiovascular Disease|volume=7|issue=4|pages=301–8|year=1997}}</ref> |
|||
====Intermittent claudication (IC)==== |
|||
A study found that moderate consumption of alcohol had a protective effect against [[intermittent claudication]]. The lowest risk was seen in men who drank 1 to 2 drinks per day and in women who drank half to 1 drink per day.<ref>{{cite journal|author=Djoussé L, Levy D, Murabito JM, Cupples LA, Ellison RC|title=Alcohol consumption and risk of intermittent claudication in the Framingham Heart Study|journal=Circulation|volume=102|issue=25|pages=3092–7|date=19 December 2000|pmid=11120700|url=http://circ.ahajournals.org/cgi/content/full/102/25/3092}}</ref> |
|||
====Heart attack and stroke==== |
|||
Drinking in moderation has been found to help those who have suffered a [[heart attack]] survive it.<ref>{{cite journal|url=http://www.ncbi.nlm.nih.gov/pubmed/9863785|author=Muntwyler J, Hennekens CH, Buring JE, Gaziano JM|title=Mortality and light to moderate alcohol consumption after myocardial infarction|journal=Lancet|volume=352|issue=9144|pages=1882–5|year=1998|month=December|pmid=9863785|doi=10.1016/S0140-6736(98)06351-X}}</ref><ref>{{cite journal|author=Mukamal KJ, Maclure M, Muller JE, Sherwood JB, Mittleman MA|title=Prior alcohol consumption and mortality following acute myocardial infarction|journal=JAMA|volume=285|issue=15|pages=1965–70|year=2001|month=April|pmid=11308432|url=http://jama.ama-assn.org/cgi/pmidlookup?view=long&pmid=11308432|doi=10.1001/jama.285.15.1965}}</ref><ref>[http://www.newswise.com/articles/view/506828/ Alcohol helps reduce damage after heart attacks]</ref> However, excessive alcohol consumption leads to an increased risk of [[heart failure]].<ref>{{cite journal|author=Djoussé L, Gaziano JM|title=Alcohol consumption and heart failure: a systematic review|journal=Curr Atheroscler Rep|volume=10|issue=2|pages=117–20|year=2008|month=April|pmid=18417065|doi=10.1007/s11883-008-0017-z|pmc=2365733}}</ref> A review of the literature found that half a drink of alcohol offered the best level of protection. However, they noted that at present there have been no randomised trials to confirm the evidence which suggests a protective role of low doses of alcohol against heart attacks.<ref>{{cite journal|author=Kloner RA, Rezkalla SH|title=To drink or not to drink? That is the question|journal=Circulation|volume=116|issue=11|pages=1306–17|year=2007|month=September|pmid=17846344|doi=10.1161/CIRCULATIONAHA.106.678375|url=http://circ.ahajournals.org/cgi/content/full/116/11/1306}}</ref> However, moderate alcohol consumption is associated with hypertension.<ref name="Andréasson-"/> There is an increased risk of [[hypertriglyceridemia]], [[cardiomyopathy]], [[hypertension]], and [[stroke]] if 3 or more [[standard drink]]s of alcohol are taken per day.<ref>{{cite journal|author=Saremi A, Arora R|title=The cardiovascular implications of alcohol and red wine|journal=Am J Ther|volume=15|issue=3|pages=265–77|year=2008|pmid=18496264|doi=10.1097/MJT.0b013e3180a5e61a}}</ref> |
|||
====Cardiomyopathy==== |
|||
Large amount of alcohol over the long term can lead to alcoholic [[cardiomyopathy]]. Alcoholic cardiomyopathy presents in a manner clinically identical to idiopathic [[dilated cardiomyopathy]], involving hypertrophy of the musculature of the heart that can lead to congestive heart failure.<ref name="Awtry-">{{Cite journal|last1=Awtry|first1=EH.|last2=Philippides|first2=GJ.|title=Alcoholic and cocaine-associated cardiomyopathies.|journal=Prog Cardiovasc Dis|volume=52|issue=4|pages=289–99|year=2010|doi=10.1016/j.pcad.2009.11.004|pmid=20109599}}</ref> |
|||
====Hematologic diseases==== |
|||
Alcoholics may have [[anemia]] from several causes;<ref>{{cite journal|author=Savage D, Lindenbaum J|title=Anemia in alcoholics|journal=Medicine (Baltimore)|volume=65|issue=5|pages=322–38|year=1986|pmid=3747828}}</ref> they may also develop [[thrombocytopenia]] from direct toxic effect on [[megakaryocytes]], or from [[hypersplenism]]. |
|||
===Nervous system=== |
|||
[[File:HarmCausedByDrugsTable.svg|thumb|Results of the [[#ISCD|ISCD]] 2010 study ranking the levels of damage caused by drugs, in the opinion of drug-harm experts. When harm to self and others is summed, alcohol was the most harmful of all drugs considered, scoring 72%.]] |
|||
Chronic heavy alcohol consumption impairs brain development, causes [[brain shrinkage]], [[dementia]], [[physical dependence]], increases neuropsychiatric and cognitive disorders and causes distortion of the [[brain chemistry]]. Some studies however have shown that moderate alcohol consumption may decrease risk of dementia, including Alzheimer disease, although there are studies which find the opposite. At present, due to poor study design and methodology, the literature is inconclusive on whether moderate alcohol consumption increases the risk of dementia or decreases it.<ref>{{cite journal|author=Panza F, Capurso C, D'Introno A, ''et al.''|title=Vascular risk factors, alcohol intake, and cognitive decline|journal=J Nutr Health Aging|volume=12|issue=6|pages=376–81|year=2008|pmid=18548174|doi=10.1007/BF02982669}}</ref> Evidence for a protective effect of low to moderate alcohol consumption on age related cognitive decline and dementia has been suggested by some research, however, other research has not found a protective effect of low to moderate alcohol consumption.<ref name="Panza-2009">{{Cite journal|last1=Panza|first1=F.|last2=Capurso|first2=C.|last3=D'Introno|first3=A.|last4=Colacicco|first4=AM.|last5=Frisardi|first5=V.|last6=Lorusso|first6=M.|last7=Santamato|first7=A.|last8=Seripa|first8=D.|last9=Pilotto|first9=A.|title=Alcohol drinking, cognitive functions in older age, predementia, and dementia syndromes.|journal=J Alzheimers Dis|volume=17|issue=1|pages=7–31|month=May|year=2009|doi=10.3233/JAD-2009-1009|pmid=19494429}}</ref> Some evidence suggests that low to moderate alcohol consumption may speed up brain volume loss.<ref name="Verbaten-2009">{{Cite journal|last1=Verbaten|first1=MN.|title=Chronic effects of low to moderate alcohol consumption on structural and functional properties of the brain: beneficial or not?|journal=Hum Psychopharmacol|volume=24|issue=3|pages=199–205|month=Apr|year=2009|doi=10.1002/hup.1022|pmid=19330800}}</ref> Chronic consumption of alcohol may result in increased plasma levels of the toxic amino acid [[homocysteine]];<ref>{{cite journal|pmid=11373253|volume=36|issue=3|title=Moderate alcohol consumption in social drinkers raises plasma homocysteine levels: a contradiction to the 'French Paradox'?|year=2001|author=Bleich S, Bleich K, Kropp S, ''et al.''|journal=Alcohol Alcohol.|pages=189–92}}</ref><ref>{{cite journal|pmid=15770107|volume=29|issue=3|title=Evidence of increased homocysteine levels in alcoholism: the Franconian alcoholism research studies (FARS)|year=2005|month=March|author=Bleich S, Carl M, Bayerlein K, ''et al.''|journal=Alcohol. Clin. Exp. Res.|pages=334–6}}</ref> which may explain alcohol withdrawal seizures,<ref>{{cite journal|pmid=10976956|volume=11|issue=12|title=Plasma homocysteine is a predictor of alcohol withdrawal seizures|year=2000|month=August|author=Bleich S, Degner D, Bandelow B, von Ahsen N, Rüther E, Kornhuber J|journal=NeuroReport|pages=2749–52}}</ref> alcohol-induced brain atrophy<ref>{{cite journal|pmid=12531462|volume=335|issue=3|title=Hyperhomocysteinemia as a new risk factor for brain shrinkage in patients with alcoholism|year=2003|month=January|author=Bleich S, Bandelow B, Javaheripour K, ''et al.''|journal=Neurosci. Lett.|pages=179–82|doi=10.1016/S0304-3940(02)01194-1}}</ref> and alcohol-related cognitive disturbances.<ref>{{cite journal|pmid=15997414|doi=10.1007/s00702-005-0333-1|volume=113|issue=3|title=Short-term cognition deficits during early alcohol withdrawal are associated with elevated plasma homocysteine levels in patients with alcoholism|year=2006|month=March|author=Wilhelm J, Bayerlein K, Hillemacher T, ''et al.''|journal=J Neural Transm|pages=357–63}}</ref> Alcohol's impact on the nervous system can also include disruptions of [[memory]] and [[learning]] (''see [[Effects of alcohol on memory#Effects on nervous system|Effects of alcohol on memory]]''), such as resulting in a [[Blackout (alcohol-related amnesia)|blackout phenomenon]]. |
|||
====Strokes==== |
|||
Epidemiological studies of middle-aged populations generally find the relationship between alcohol intake and the risk of stroke to be either U- or J-shaped.<ref name="Di Castelnuovo-2009">{{Cite journal|last1=Di Castelnuovo|first1=A.|last2=Costanzo|first2=S.|last3=di Giuseppe|first3=R.|last4=de Gaetano|first4=G.|last5=Iacoviello|first5=L.|title=Alcohol consumption and cardiovascular risk: mechanisms of action and epidemiologic perspectives.|journal=Future Cardiol|volume=5|issue=5|pages=467–77|month=Sep|year=2009|doi=10.2217/fca.09.36|PMID=19715411}}</ref><ref name="Klatsky-2009">{{Cite journal|last1=Klatsky|first1=AL.|title=Alcohol and cardiovascular diseases.|journal=Expert Rev Cardiovasc Ther|volume=7|issue=5|pages=499–506|month=May|year=2009|doi=10.1586/erc.09.22|PMID=19419257}}</ref><ref name="Galimanis-2009">{{Cite journal|last1=Galimanis|first1=A.|last2=Mono|first2=ML.|last3=Arnold|first3=M.|last4=Nedeltchev|first4=K.|last5=Mattle|first5=HP.|title=Lifestyle and stroke risk: a review.|journal=Curr Opin Neurol|volume=22|issue=1|pages=60–8|month=Feb|year=2009|doi=10.1097/WCO.0b013e32831fda0e|PMID=19155763}}</ref><ref name="O'Keefe-2007">{{Cite journal|last1=O'Keefe|first1=JH.|last2=Bybee|first2=KA.|last3=Lavie|first3=CJ.|title=Alcohol and cardiovascular health: the razor-sharp double-edged sword|journal=J Am Coll Cardiol|volume=50|issue=11|pages=1009–14|month=Sep|year=2007|doi=10.1016/j.jacc.2007.04.089|PMID=17825708}}</ref> There may be very different effects of alcohol based on the type of stroke studied. The predominate form of stroke in Western cultures is ischemic, whereas non-western cultures have more hemorrhagic stroke. In contrast to the beneficial effect of alcohol on ischemic stroke, consumption of more than 2 drinks per day increases the risk of hemorrhagic stroke. The National Stroke Association estimates this higher amount of alcohol increases stroke risk by 50%.<ref>http://www.stroke.org/site/PageServer?pagename=Alcohol</ref> "For stroke, the observed relationship between alcohol consumption and risk in a given population depends on the proportion of strokes that are hemorrhagic. Light-to-moderate alcohol intake is associated with a lower risk of ischemic stroke which is likely to be, in part, causal. Hemorrhagic stroke, on the other hand, displays a loglinear relationship with alcohol intake."<ref name="Emberson-2006">{{Cite journal|last1=Emberson|first1=JR.|last2=Bennett|first2=DA.|title=Effect of alcohol on risk of coronary heart disease and stroke: causality, bias, or a bit of both?|journal=Vasc Health Risk Manag|volume=2|issue=3|pages=239–49|year=2006|PMID=17326330|pmc=1993990}}</ref> |
|||
====Brain==== |
|||
Alcohol abuse is associated with widespread and significant brain [[lesion]]s. Alcohol related brain damage is not only due to the direct toxic effects of alcohol; alcohol withdrawal, nutritional deficiency, electrolyte disturbances, and liver damage are also believed to contribute to alcohol-related brain damage.<ref name="Neiman-1998">{{Cite journal|doi=10.1111/j.1530-0277.1998.tb04389.x|last1=Neiman|first1=J.|title=Alcohol as a risk factor for brain damage: neurologic aspects|journal=Alcohol Clin Exp Res|volume=22|issue=7 Suppl|pages=346S–351S|month=Oct|year=1998|pmid=9799959}}</ref> The long-term effects of alcohol on brain chemistry is an important cause of [[Fatigue (medical)#Chronic fatigue|chronic fatigue]].<ref name="Avellaneda Fernández-2009">{{Cite journal|last1=Avellaneda Fernández|first1=A.|last2=Pérez Martín|first2=A.|last3=Izquierdo Martínez|first3=M.|last4=Arruti Bustillo|first4=M.|last5=Barbado Hernández|first5=FJ.|last6=de la Cruz Labrado|first6=J.|last7=Díaz-Delgado Peñas|first7=R.|last8=Gutiérrez Rivas|first8=E.|last9=Palacín Delgado|first9=C.|title=Chronic fatigue syndrome: aetiology, diagnosis and treatment.|journal=BMC Psychiatry|volume=9 Suppl 1|pages=S1|year=2009|doi=10.1186/1471-244X-9-S1-S1|PMID=19857242}}</ref> |
|||
=====Adolescent brain development===== |
|||
Consuming large amounts of alcohol over a period of time can impair normal brain development in humans.<ref>{{cite journal|author=Tapert SF, Brown GG, Kindermann SS, Cheung EH, Frank LR, Brown SA|title=fMRI measurement of brain dysfunction in alcohol-dependent young women|journal=[[Alcohol. Clin. Exp. Res.]]|volume=25|issue=2|pages=236–45|year=2001|month=February|pmid=11236838 |doi=10.1111/j.1530-0277.2001.tb02204.x|url=http://www3.interscience.wiley.com/resolve/openurl?genre=article&sid=nlm:pubmed&issn=0145-6008&date=2001&volume=25&issue=2&spage=236}}</ref> Deficits in retrieval of verbal and nonverbal information and in visuospatial functioning were evident in youths with histories of heavy drinking during early and middle adolescence.<ref>{{cite journal|author=Squeglia LM, Jacobus J, Tapert SF|title=The influence of substance use on adolescent brain development|journal=Clin EEG Neurosci|volume=40|issue=1|pages=31–8|year=2009|month=January|pmid=19278130|pmc=2827693}}</ref><ref>{{cite journal|author=Brown SA, Tapert SF, Granholm E, Delis DC|title=Neurocognitive functioning of adolescents: effects of protracted alcohol use|journal=[[Alcohol Clin Exp Res]].|volume=24|issue=2|pages=164–71|year=2000|month=February|pmid=10698367|doi=10.1111/j.1530-0277.2000.tb04586.x|url=http://www3.interscience.wiley.com/resolve/openurl?genre=article&sid=nlm:pubmed&issn=0145-6008&date=2000&volume=24&issue=2&spage=164}}</ref> |
|||
During adolescence critical stages of neurodevelopment occur, including remodeling and functional changes in [[synaptic plasticity]] and neuronal connectivity in different brain regions. These changes may make adolescents especially susceptible to the harmful effects of alcohol. Compared to adults, adolescents exposed to alcohol are more likely to exhibit cognitive deficits (including learning and memory dysfunction). Some of these cognitive effects, such as learning impairments, may persist into adulthood.<ref>{{cite pmid|20113871}}</ref> |
|||
=====Mechanisms of action===== |
|||
======Neuroinflammation====== |
|||
Ethanol can trigger the activation of [[astrocyte|astroglial cells]] which can produce a proinflammatory response in the brain. Ethanol interacts with the [[TLR4]] and [[Interleukin 1 receptor, type I|IL-1RI]] receptors on these cells to activate intracellular signal transduction pathways. Specifically, ethanol induces the phosphorylation of IL-1R-associated kinase (IRAK), [[Extracellular signal-regulated kinases|ERK1/2]], stress-activated protein kinase (SAPK)/[[c-Jun N-terminal kinases|JNK]], and [[p38 mitogen-activated protein kinases|p38 mitogen-activated protein kinase (p38 MAPK)]]. Activation of the IRAK/MAPK pathway leads to the stimulation of the [[transcription factor]]s [[NF-kappaB]] and [[AP-1 transcription factor|AP-1]]. These transcription factors cause the upregulation of [[Nitric oxide synthase|inducible nitric oxide synthase (iNOS)]] and [[PTGS2|cyclooxygenase-2 (COX-2)]] expression.<ref name="pmid16272348">{{cite pmid|16272348}}</ref> The upregulation of these inflammatory mediators by ethanol is also associated with an increase in [[caspase 3]] activity and a corresponding increase in cell [[apoptosis]].<ref name="pmid16272348"/><ref>{{cite pmid|17284196}}</ref> The exact mechanism by which various concentrations of ethanol either activates or inhibits TLR4/IL-1RI signaling is not currently known, though it may involve alterations in [[lipid raft]] clustering <ref>{{cite pmid|18061674}}</ref> or [[cell adhesion]] complexes and actin [[cytoskeleton]] organization.<ref>{{cite pmid|12704810}}</ref> |
|||
======Changes in dopaminergic and glutamatergic signaling pathways====== |
|||
Intermittent ethanol treatment causes a decrease in expression of the [[dopamine receptor]] type 2 (D2R) and a decrease in phosphorylation of 2B subunit of the [[NMDA receptor]] (NMDAR2B) in the [[prefrontal cortex]], [[hippocampus]], [[nucleus accumbens]], and for only D2R the [[striatum]]. It also causes changes in the acetylation of [[histone]]s H3 and H4 in the prefrontal cortex, nucleus accumbens, and striatum, suggesting [[chromatin]] remodeling changes which may mediate long-term alterations. Additionally, adolescent rats pre-exposed to ethanol have higher basal levels of dopamine in the nucleus accumbens, along with a prolonged dopamine response in this area in response to a challenge dose of ethanol. Together, these results suggest that alcohol exposure during adolescence can sensitize the [[Mesolimbic pathway|mesolimbic]] and [[Mesocortical pathway|mesocortical]] dopamine pathways to cause changes in [[dopaminergic]] and glutamatergic signaling, which may affect the remodeling and functions of the adolescent brain.<ref>{{cite pmid|19077056}}</ref> These changes are significant as alcohol’s effect on NMDARs could contribute to learning and memory dysfunction (''see [[Effects of alcohol on memory#Effects on nervous system|Effects of alcohol on memory]]''). |
|||
======Inhibition of hippocampal neurogenesis====== |
|||
Excessive alcohol intake ([[binge drinking]]) causes a decrease in hippocampal [[neurogenesis]], via decreases in neural stem cell proliferation and newborn cell survival.<ref name="pmid19554644">{{cite pmid|19554644}}</ref><ref name="pmid20534463">{{cite pmid|20534463}}</ref> Alcohol decreases the number of cells in S-phase of the [[cell cycle]], and may arrest cells in the G1 phase, thus inhibiting their proliferation.<ref name="pmid19554644"/> Ethanol has different effects on different types of actively dividing hippocampal progenitors during their initial phases of neuronal development. Chronic alcohol exposure decreases the number of proliferating cells that are [[Radial glial cell|radial glia]]-like, preneuronal, and intermediate types, while not affecting early neuronal type cells; suggesting ethanol treatment alters the precursor cell pool. Furthermore, there is a greater decrease in differentiation and immature neurons than there is in proliferating progenitors, suggesting that the abnormal decrease in the percentage of actively dividing preneuronal progenitors results in a greater reduction in the maturation and survival of postmitotic cells.<ref name="pmid20534463"/> |
|||
Additionally, alcohol exposure increased several markers of cell death. In these studies neural degeneration seems to be mediated by non-apoptotic pathways.<ref name="pmid19554644"/><ref name="pmid20534463"/> One of the proposed mechanisms for alcohol’s neurotoxicity is the production of nitric oxide (NO), yet other studies have found alcohol-induced NO production to lead to apoptosis (''see [[#Neuroinflammation|Neuroinflammation]] section''). |
|||
====Cognition and dementia==== |
|||
Excessive alcohol intake is associated with impaired [[prospective memory]]. This impaired cognitive ability leads to increased failure to carry out an intended task at a later date, for example, forgetting to lock the door or to post a letter on time. The higher the volume of alcohol consumed and the longer consumed, the more severe the impairments.<ref name="Heffernan-2008">{{Cite journal|doi=10.2174/1874473710801010036|last1=Heffernan|first1=TM.|title=The impact of excessive alcohol use on prospective memory: a brief review.|journal=Curr Drug Abuse Rev|volume=1|issue=1|pages=36–41|month=Jan|year=2008|pmid=19630703}}</ref> One of the organs most sensitive to the toxic effects of chronic alcohol consumption is the brain. In France approximately 20% of admissions to mental health facilities are related to alcohol-related cognitive impairment, most notably alcohol-related dementia. Chronic excessive alcohol intake is also associated with serious cognitive decline and a range of neuropsychiatric complications. The elderly are the most sensitive to the toxic effects of alcohol on the brain.<ref>{{cite journal|author=Pierucci-Lagha A, Derouesné C|title=[Alcoholism and aging. 2. Alcoholic dementia or alcoholic cognitive impairment?]|language=French|journal=Psychol Neuropsychiatr Vieil|volume=1|issue=4|pages=237–49|year=2003|month=December|pmid=15683959}}</ref> There is some inconclusive evidence that small amounts of alcohol taken in earlier adult life is protective in later life against cognitive decline and dementia.<ref>{{cite journal|author=Peters R, Peters J, Warner J, Beckett N, Bulpitt C|title=Alcohol, dementia and cognitive decline in the elderly: a systematic review|journal=Age Ageing|volume=37|issue=5|pages=505–12|year=2008|month=September|pmid=18487267|doi=10.1093/ageing/afn095|url=http://ageing.oxfordjournals.org/cgi/content/full/37/5/505}}</ref> However, a study concluded, "Our findings suggest that, despite previous suggestions, moderate alcohol consumption does not protect older people from cognitive decline."<ref>Claudia Cooper, Paul Bebbington, Howard Meltzer, Rachel Jenkins, Traolach Brugha, James Lindesay and Gill Livingston [http://jnnp.bmj.com/cgi/content/abstract/jnnp.2008.163964v1 Alcohol in moderation, premorbid intelligence and cognition In Older Adults: results from the Psychiatric Morbidity Survey] ''J Neurol Neurosurg Psychiatry'' {{doi|10.1136/jnnp.2008.163964}}</ref> |
|||
[[Acetaldehyde]] is produced from ethanol metabolism by the liver. The acetaldehyde is further metabolized by the enzyme acetaldehyde dehydrognease. A deficency of this enzyme is not uncommon in individuals from Northeastern Asia as pointed out in a study from Japan.<ref name=ohta>{{cite journal|last=|first=S|authorlink=Ohta|coauthors=Ohsawa I, Kamino K, Ando F, Shimokata H.|year=2004|month=April|title=Mitochondrial ALDH2 Deficiency as an Oxidative Stress|journal=Annals of the New York Academy of Sciences|volume=1011|pages=36–44|url=http://www3.interscience.wiley.com/journal/118765604/abstract?CRETRY=1&SRETRY=0|accessdate=2009-08-13|doi=10.1196/annals.1293.004|pmid=15126281|last1=Ohta}}</ref> This study has suggested these individuals may be more susceptible to late-onset [[Alzheimer's disease]], however this higher risk is associated with the enzyme deficiency not with alcohol consumption. Individuals with this defect generally do not drink alcohol. |
|||
[[Wernicke-Korsakoff syndrome]] is a manifestation of [[thiamine]] deficiency, usually as a secondary effect of alcohol abuse.<ref>{{cite journal|author=Martin PR, Singleton CK, Hiller-Sturmhöfel S|title=The role of thiamine deficiency in alcoholic brain disease|journal=Alcohol Res Health|volume=27|issue=2|pages=134–42|year=2003|pmid=15303623}}</ref> The syndrome is a combined manifestation of two eponymous disorders, [[Korsakoff's syndrome|Korsakoff's Psychosis]] and [[Wernicke's encephalopathy]], named after Drs. [[Sergei Korsakoff]] and [[Carl Wernicke]]. Wernicke's encephalopathy is the acute presentation of the syndrome and is characterised by a [[confusion]]al state while Korsakoff's psychosis main symptoms are [[amnesia]] and [[executive functions|executive dysfunction]].<ref>{{cite journal|author=Butters N|title=The Wernicke-Korsakoff syndrome: a review of psychological, neuropathological and etiological factors|journal=Curr Alcohol|volume=8|pages=205–32|year=1981|pmid=6806017}}</ref> |
|||
====Essential tremor==== |
|||
[[Essential tremor]]s can be temporarily relieved in up to two-thirds of patients by drinking small amounts of alcohol.<ref> |
|||
{{cite journal|author=Bain PG, Findley LJ, Thompson PD, ''et al.''|title=A study of hereditary essential tremor|journal=Brain|volume=117|issue=(Pt 4)|pages=805–24|year=1994|month=August|pmid=7922467|doi=10.1093/brain/117.4.805|url=http://brain.oxfordjournals.org/cgi/pmidlookup?view=long&pmid=7922467}}<br /> |
|||
{{cite journal|author=Lou JS, Jankovic J|title=Essential tremor: clinical correlates in 350 patients|journal=Neurology|volume=41|issue=2 (Pt 1)|pages=234–8|year=1991|month=February|pmid=1992367}}<br /> |
|||
{{cite journal|doi=10.1002/mds.870131316|author=Wasielewski PG, Burns JM, Koller WC|title=Pharmacologic treatment of tremor|journal=Mov Disord.|volume=13|issue=Suppl 3|pages=90–100|year=1998|pmid=9827602}}<br /> |
|||
{{cite journal|author=Boecker H, Wills AJ, Ceballos-Baumann A, ''et al.''|title=The effect of ethanol on alcohol-responsive essential tremor: a positron emission tomography study|journal=Ann. Neurol.|volume=39|issue=5|pages=650–8|year=1996|month=May|pmid=8619551|doi=10.1002/ana.410390515}}<br /> |
|||
{{cite journal|title=Setting a steady course for benign essential tremor|journal=Johns Hopkins Med Lett Health After 50|volume=11|issue=10|pages=3|year=1999|month=December|pmid=10586714}}</ref> |
|||
Ethanol is known to activate aminobutyric acid type A (GABAA) and inhibit N-methyl-D-aspartate (NMDA) glutamate receptors, which are both implicated in essential tremor pathology <ref>{{cite pmid|20721919}}</ref> and could underlie the ameliorative effects.<ref>{{cite pmid|21640732}}</ref><ref>{{cite pmid|17366267}}</ref> Additionally, the effects of ethanol have been studied in different animal essential tremor models. |
|||
''For more details on this topic, see [[Essential tremor#Essential Tremor Models|Essential tremor]]'' |
|||
====Sleep==== |
|||
Chronic use of alcohol used to induce sleep can lead to [[insomnia]]. Frequent moving between sleep stages occurs, with awakenings due to headaches and [[diaphoresis]]. Stopping chronic alcohol abuse can also lead to profound disturbances of sleep with vivid dreams. Chronic alcohol abuse is associated with [[NREM]] stage 3 and 4 sleep as well as suppression of [[REM sleep]] and REM sleep fragmentation. During withdrawal REM sleep is typically exaggerated as part of a [[rebound effect]].<ref name="sleep_medicine_a04">{{Cite book|last1=Lee-chiong|first1=Teofilo|title=Sleep Medicine: Essentials and Review|date=24 April 2008|publisher=Oxford University Press, USA|url=http://books.google.com/?id=s1F_DEbRNMcC&pg=PT105|isbn=0-19-530659-7|page=105}}</ref> |
|||
====Mental health effects==== |
|||
High rates of [[major depressive disorder]] occur in heavy drinkers and those who abuse alcohol. Whether it is more true that major depressive disorder causes self-medicating alcohol abuse, or the increased incidence of the disorder in alcohol abusers is caused by the drinking, is not known though some evidence suggests drinking causes the disorder.<ref>{{cite journal|author=Fergusson DM, Boden JM, Horwood LJ|title=Tests of causal links between alcohol abuse or dependence and major depression|journal=Arch. Gen. Psychiatry|volume=66|issue=3|pages=260–6|year=2009|month=March|pmid=19255375|doi=10.1001/archgenpsychiatry.2008.543|url=http://archpsyc.ama-assn.org/cgi/pmidlookup?view=long&pmid=19255375}}</ref> Alcohol misuse is associated with a number of mental health disorders and alcoholics have a very high [[suicide]] rate.<ref>{{cite journal|author=Chignon JM, Cortes MJ, Martin P, Chabannes JP|title=[Attempted suicide and alcohol dependence: results of an epidemiologic survey]|language=French|journal=Encephale|volume=24|issue=4|pages=347–54|year=1998|pmid=9809240}}</ref> A study of people hospitalised for suicide attempts found that those who were alcoholics were 75 times more likely to go on to successfully commit suicide than non-alcoholic suicide attempters.<ref>{{Cite book|last1=Ayd|first1=Frank J.|title=Lexicon of psychiatry, neurology, and the neurosciences|url=http://books.google.com/?id=ea_QVG2BFy8C|date=31 May 2000|publisher=Lippincott-Williams Wilkins|location=Philadelphia|isbn=978-0-7817-2468-5|page=349}}</ref> In the general alcoholic population the increased risk of suicide compared to the general public is 5-20 times greater. About 15 percent of alcoholics commit suicide. Abuse of other drugs is also associated with an increased risk of suicide. About 33 percent of suicides in the under 35s are due to alcohol or other substance misuse.<ref>{{Cite book|last1=Appleby|first1=Louis|last2=Duffy|first2=David|last3=Ryan|first3=Tony|date=25 Aug 2004|title=New Approaches to Preventing Suicide: A Manual For Practitioners|url=http://books.google.com/?id=d6Kw9GaJdzEC|publisher=Jessica Kingsley Publishers|isbn=978-1-84310-221-2|pages=31–32}}</ref> |
|||
[[Social skills]] are significantly impaired in people suffering from alcoholism due to the neurotoxic effects of alcohol on the brain, especially the [[prefrontal cortex]] area of the brain. The social skills that are impaired by [[alcohol abuse]] include impairments in perceiving facial emotions, prosody perception problems and [[theory of mind]] deficits; the ability to understand humour is also impaired in alcohol abusers.<ref name="pmid18412750">{{cite journal|author=Uekermann J, Daum I|title=Social cognition in alcoholism: a link to prefrontal cortex dysfunction?|journal=Addiction|volume=103|issue=5|pages=726–35|year=2008|month=May|pmid=18412750|doi=10.1111/j.1360-0443.2008.02157.x}}</ref> |
|||
Studies have shown that alcohol dependence relates directly to [[Craving (withdrawal)|cravings]] and [[irritability]].<ref>{{cite journal|author=Jasova D, Bob P, Fedor-Freybergh P|title=Alcohol craving, limbic irritability, and stress|journal=Med Sci Monit.|volume=13|issue=12|pages=CR543–7|year=2007|month=December|pmid=18049433|url=http://www.medscimonit.com/fulltxt.php?ICID=563763|accessdate=2008-05-13}}</ref> Another study has shown that alcohol use is a significant predisposing factor towards [[antisocial behavior]] in children.<ref name=antisocial>{{cite journal|author=Young R, Sweeting H, West P|title=A longitudinal study of alcohol use and antisocial behaviour in young people|journal=Alcohol Alcohol.|volume=43|issue=2|pages=204–14|year=2008|pmid=17977868|doi=10.1093/alcalc/agm147|url=http://alcalc.oxfordjournals.org/cgi/pmidlookup?view=long&pmid=17977868|accessdate=2008-05-13|pmc=2367698}}</ref> Depression, anxiety and panic disorder are disorders commonly reported by alcohol dependent people. Alcoholism is associated with dampened activation in brain networks responsible for emotional processing (''e.g.'' the [[amygdala]] and [[hippocampus]]).<ref>{{cite journal|author=Marinkovic K|coauthors=Oscar-Berman M, Urban T, O'Reilly CE, Howard JA, Sawyer K, Harris GJ|year=2009|month=November|title=Alcoholism and dampened temporal limbic activation to emotional faces|journal=Alcohol Clin Exp Res|volume=33|issue=11|pages=1880–92|pmid=19673745|doi=10.1111/j.1530-0277.2009.01026.x}}</ref> Evidence that the mental health disorders are often induced by alcohol misuse via distortion of brain neurochemistry is indicated by the improvement or disappearance of symptoms that occurs after prolonged abstinence, although problems may worsen in early withdrawal and recovery periods.<ref>{{cite journal|author=Wetterling T|coauthors=Junghanns K|year=2000|month=December|title=Psychopathology of alcoholics during withdrawal and early abstinence|journal=Eur Psychiatry|volume=15|issue=8|pages=483–8|pmid=11175926|doi=10.1016/S0924-9338(00)00519-8}}</ref><ref>{{cite journal|author=Cowley DS|year=1992|month=January|date=24|title=Alcohol abuse, substance abuse, and panic disorder|journal=Am J Med|volume=92|issue=1A|pages=41S–8S|pmid=1346485|doi=10.1016/0002-9343(92)90136-Y}}</ref><ref>{{cite journal|author=Cosci F|coauthors=Schruers KR, Abrams K, Griez EJ|year=2007|month=June|title=Alcohol use disorders and panic disorder: a review of the evidence of a direct relationship|journal=J Clin Psychiatry|volume=68|issue=6|pages=874–80|pmid=17592911|doi=10.4088/JCP.v68n0608}}</ref> Psychosis is secondary to several alcohol-related conditions including acute intoxication and withdrawal after significant exposure.<ref name=emedicine>{{EMedicine|med|3113|Alcohol-Related Psychosis}}</ref> Chronic alcohol misuse can cause psychotic type symptoms to develop, more so than with other drugs of abuse. Alcohol abuse has been shown to cause an 800% increased risk of psychotic disorders in men and a 300% increased risk of psychotic disorders in women which are not related to pre-existing psychiatric disorders. This is significantly higher than the increased risk of psychotic disorders seen from cannabis use making alcohol abuse a very significant cause of psychotic disorders.<ref>{{cite journal|author=Tien AY, Anthony JC|title=Epidemiological analysis of alcohol and drug use as risk factors for psychotic experiences|journal=J. Nerv. Ment. Dis.|volume=178|issue=8|pages=473–80|year=1990|month=August|pmid=2380692|doi=10.1097/00005053-199017880-00001}}</ref> Approximately 3 percent of people who are alcohol dependent experience psychosis during acute intoxication or withdrawal. Alcohol-related psychosis may manifest itself through a [[kindling (sedative-hypnotic withdrawal)|kindling mechanism]]. The mechanism of alcohol-related psychosis is due to distortions to neuronal membranes, [[gene expression]], as well as [[thiamin]] deficiency. It is possible in some cases that alcohol abuse via a kindling mechanism can cause the development of a chronic substance-induced psychotic disorder, i.e. [[schizophrenia]]. The effects of an alcohol-related psychosis include an increased risk of depression and suicide as well as psychosocial impairments.<ref name=emedicine/> |
|||
While [[ethanol|alcohol]] initially helps social phobia or panic symptoms, with longer term alcohol misuse can often worsen social phobia symptoms and can cause panic disorder to develop or worsen, during alcohol intoxication and especially during the [[alcohol withdrawal syndrome]]. This effect is not unique to alcohol but can also occur with long term use of drugs which have a similar mechanism of action to alcohol such as the [[benzodiazepines]] which are sometimes prescribed as tranquillisers to people with alcohol problems.<ref>{{cite journal|author=Terra MB, Figueira I, Barros HM|title=Impact of alcohol intoxication and withdrawal syndrome on social phobia and panic disorder in alcoholic inpatients|journal=Rev Hosp Clin Fac Med Sao Paulo|volume=59|issue=4|pages=187–92|year=2004|month=August|pmid=15361983|url=http://www.scielo.br/scielo.php?script=sci_arttext&pid=S0041-87812004000400006&lng=en&nrm=iso&tlng=en|doi=10.1590/S0041-87812004000400006}}</ref> Approximately half of patients attending mental health services for conditions including [[anxiety disorders]] such as [[panic disorder]] or [[social anxiety disorder|social phobia]] suffer from alcohol or [[benzodiazepine dependence]]. It was noted that every individual has an individual sensitivity level to alcohol or sedative hypnotic drugs and what one person can tolerate without ill health another will suffer very ill health and that even moderate drinking can cause [[rebound anxiety]] syndromes and sleep disorders. A person who is suffering the toxic effects of alcohol will not benefit from other therapies or medications as they do not address the root cause of the symptoms.<ref>{{cite journal|author=Cohen SI|title=Alcohol and benzodiazepines generate anxiety, panic and phobias|journal=J R Soc Med|volume=88|issue=2|pages=73–7|year=1995|month=February|pmid=7769598|pmc=1295099}}</ref> |
|||
===Digestive system and weight gain=== |
|||
{{see also|Alcohol and weight|Alcoholic liver disease|Alcoholic hepatitis|Fatty liver|Cirrhosis}} |
|||
The impact of alcohol on weight-gain is contentious: some studies find no effect,<ref>{{cite journal|author=Cordain L, Bryan ED, Melby CL, Smith MJ|title=Influence of moderate daily wine consumption on body weight regulation and metabolism in healthy free-living males|journal=J Am Coll Nutr|volume=16|issue=2|pages=134–9|date=1 April 1997|pmid=9100213|url=http://intl.jacn.org/cgi/content/abstract/16/2/134}}</ref> others find decreased<ref>{{cite journal|author=Arif AA, Rohrer JE|title=Patterns of alcohol drinking and its association with obesity: data from the Third National Health and Nutrition Examination Survey, 1988-1994|journal=BMC Public Health|volume=5|pages=126|year=2005|pmid=16329757|pmc=1318457|doi=10.1186/1471-2458-5-126|url=http://www.biomedcentral.com/1471-2458/5/126}}</ref> or increased effect on weight gain. |
|||
Alcohol use increases the risk of chronic [[gastritis]] (stomach inflammation);<ref>{{cite journal|author=[[National Institute on Alcohol Abuse and Alcoholism]] (NIAAA)|title=Health risks and benefits of alcohol consumption|journal=Alcohol Res Health|volume=24|issue=1|pages=5–11|year=2000|pmid=11199274|url=http://pubs.niaaa.nih.gov/publications/arh24-1/05-11.pdf}}</ref><ref name=bode1>{{cite journal|author=Bode C, Bode JC|title=Alcohol's role in gastrointestinal tract disorders|journal=Alcohol Health Res World|volume=21|issue=1|pages=76–83|year=1997|pmid=15706765|url=https://webapps.ou.edu/alcohol/docs/12EtohGastroinstestinalTractDisorders76.pdf}}</ref> it is one cause of [[cirrhosis]], [[hepatitis]], and [[pancreatitis]] in both its [[Chronic pancreatitis|chronic]] and [[Acute pancreatitis|acute]] forms. |
|||
====Metabolic syndrome==== |
|||
A study concluded, "Mild to moderate alcohol consumption is associated with a lower prevalence of the [[metabolic syndrome]], with a favorable influence on lipids, waist circumference, and fasting insulin. This association was strongest among whites and among beer and wine drinkers."<ref>{{cite journal|author=Freiberg MS, Cabral HJ, Heeren TC, Vasan RS, Curtis Ellison R|title=Alcohol consumption and the prevalence of the Metabolic Syndrome in the US.: a cross-sectional analysis of data from the Third National Health and Nutrition Examination Survey|journal=Diabetes Care|volume=27|issue=12|pages=2954–9|year=2004|month=December|pmid=15562213|url=http://care.diabetesjournals.org/cgi/content/full/27/12/2954|doi=10.2337/diacare.27.12.2954}}</ref> This is also true for Asians. A J-curve association between alcohol intake and metabolic syndrome was found: "The results of the present study suggest that the metabolic syndrome is negatively associated with light alcohol consumption (1–15 g alcohol/d) in Korean adults". However, "odds ratios for the metabolic syndrome and its components tended to increase with increasing alcohol consumption."<ref>{{cite journal|author=Yoon YS, Oh SW, Baik HW, Park HS, Kim WY|title=Alcohol consumption and the metabolic syndrome in Korean adults: the 1998 Korean National Health and Nutrition Examination Survey|journal=Am. J. Clin. Nutr.|volume=80|issue=1|pages=217–24|date=1 July 2004|pmid=15213051|url=http://www.ajcn.org/cgi/content/full/80/1/217}}</ref>''' |
|||
====Gallbladder effects==== |
|||
Research has found that drinking reduces the risk of developing [[gallstones]]. Compared with alcohol abstainers, the relative risk of gallstone disease, controlling for age, sex, education, smoking, and body mass index, is 0.83 for occasional and regular moderate drinkers (< 25 ml of ethanol per day), 0.67 for intermediate drinkers (25-50 ml per day), and 0.58 for heavy drinkers. This inverse association was consistent across strata of age, sex, and body mass index."<ref>{{cite journal|author=La Vecchia C, Decarli A, Ferraroni M, Negri E|title=Alcohol drinking and prevalence of self-reported gallstone disease in the 1983 Italian National Health Survey|journal=Epidemiology|volume=5|issue=5|pages=533–6|year=1994|month=September|pmid=7986868}}</ref> Frequency of drinking also appears to be a factor. "An increase in frequency of alcohol consumption also was related to decreased risk. Combining the reports of quantity and frequency of alcohol intake, a consumption pattern that reflected frequent intake (5-7 days/week) of any given amount of alcohol was associated with a decreased risk, as compared with nondrinkers. In contrast, infrequent alcohol intake (1-2 days/week) showed no significant association with risk."<ref>{{cite journal|doi=10.1111/j.1530-0277.1999.tb04191.x|author=Leitzmann MF, Giovannucci EL, Stampfer MJ, ''et al.''|title=Prospective study of alcohol consumption patterns in relation to symptomatic gallstone disease in men|journal=Alcohol Clin Exp Res.|volume=23|issue=5|pages=835–41|year=1999|month=May|pmid=10371403|url=http://www3.interscience.wiley.com/resolve/openurl?genre=article&sid=nlm:pubmed&issn=0145-6008&date=1999&volume=23&issue=5&spage=835}}</ref> |
|||
Consumption of alcohol is unrelated to gallbladder disease.<ref>{{cite journal|author=Sahi T, Paffenbarger RS, Hsieh CC, Lee IM|title=Body mass index, cigarette smoking, and other characteristics as predictors of self-reported, physician-diagnosed gallbladder disease in male college alumni|journal=Am J Epidemiol.|volume=147|issue=7|pages=644–51|date=1 April 1998|pmid=9554603|url=http://aje.oxfordjournals.org/cgi/pmidlookup?view=long&pmid=9554603}}</ref> However one study suggested that drinkers who take [[vitamin C]] ([[ascorbic acid]]) might reduce their risk of gallbladder disease.<ref>{{cite journal|author=Simon JA, Grady D, Snabes MC, Fong J, Hunninghake DB|title=Ascorbic acid supplement use and the prevalence of gallbladder disease. Heart & Estrogen-Progestin Replacement Study (HERS) Research Group|journal=J Clin Epidemiol|volume=51|issue=3|pages=257–65|year=1998|month=March|pmid=9495691|url=http://linkinghub.elsevier.com/retrieve/pii/S0895435697802806|doi=10.1016/S0895-4356(97)80280-6}}</ref> |
|||
====Liver disease==== |
|||
[[Alcoholic liver disease]] is a major public health problem. For example in the United States up to two million people have alcohol-related liver disorders.<ref name=Barve/> Chronic alcohol abuse can cause [[fatty liver]], [[cirrhosis]] and [[alcoholic hepatitis]]. Treatment options are limited and consist of most importantly discontinuing alcohol consumption. In cases of severe liver disease, the only treatment option may be a [[liver transplant]] in alcohol abstinent patients. Research is being conducted into the effectiveness of [[anti-TNF]]s. Certain complementary medications, e.g., [[milk thistle]] and [[silymarin]], appear to offer some benefit.<ref name=Barve>{{cite journal|author=Barve A, Khan R, Marsano L, Ravindra KV, McClain C|title=Treatment of alcoholic liver disease|journal=Ann Hepatol|volume=7|issue=1|pages=5–15|year=2008|pmid=18376362|url=http://www.annalsofhepatology.com/PDF/vol7n1/Hp081-03.pdf}}</ref><ref>{{cite journal|author=Fehér J, Lengyel G|title=Silymarin in the treatment of chronic liver diseases: past and future|language=Hungarian|journal=Orv Hetil|volume=149|issue=51|pages=2413–8|year=2008|month=December|pmid=19073452|doi=10.1556/OH.2008.28519|url=http://www.akademiai.com/openurl.asp?genre=article&doi=10.1556/OH.2008.28519}}</ref> Alcohol is a leading cause of [[liver cancer]] in the Western world, accounting for 32-45% of hepatic cancers. Up to half a million people in the United States develop alcohol-related [[liver cancer]].<ref>{{cite journal|author=Voigt MD|title=Alcohol in hepatocellular cancer|journal=Clin Liver Dis|volume=9|issue=1|pages=151–69|year=2005|month=February|pmid=15763234|doi=10.1016/j.cld.2004.10.003|url=http://journals.elsevierhealth.com/retrieve/pii/S1089-3261(04)00115-1}}</ref><ref>{{cite journal|author=Morgan TR, Mandayam S, Jamal MM|title=Alcohol and hepatocellular carcinoma|journal=Gastroenterology|volume=127|issue=5 Suppl 1|pages=S87–96|year=2004|month=November|pmid=15508108|doi=10.1053/j.gastro.2004.09.020|url=http://linkinghub.elsevier.com/retrieve/pii/S0016508504015999}}</ref> Moderate alcohol consumption also increases the risk of liver disease.<ref name="Andréasson-"/> |
|||
====Pancreatitis==== |
|||
Alcohol misuse is a leading cause of both [[acute pancreatitis]] and [[chronic pancreatitis]].<ref>{{cite journal|author=Frossard JL, Steer ML, Pastor CM|title=Acute pancreatitis|journal=Lancet|volume=371|issue=9607|pages=143–52|year=2008|month=January|pmid=18191686|doi=10.1016/S0140-6736(08)60107-5|url=http://linkinghub.elsevier.com/retrieve/pii/S0140-6736(08)60107-5}}</ref><ref>{{cite journal|author=Bachmann K, Mann O, Izbicki JR, Strate T|title=Chronic pancreatitis--a surgeons' view|journal=Med. Sci. Monit.|volume=14|issue=11|pages=RA198–205|year=2008|month=November|pmid=18971885}}</ref> Chronic excessive intake of alcohol can cause destruction of the pancreas resulting in severe chronic pain, which may progress to [[pancreatic cancer]].<ref>{{cite journal|author=Nair RJ, Lawler L, Miller MR|title=Chronic pancreatitis|journal=Am Fam Physician|volume=76|issue=11|pages=1679–88|year=2007|month=December|pmid=18092710}}</ref> Chronic pancreatitis often results in [[malabsorption]] problems and [[diabetes]].<ref>{{cite journal|author=Tattersall SJ, Apte MV, Wilson JS|title=A fire inside: current concepts in chronic pancreatitis|journal=Intern Med J|volume=38|issue=7|pages=592–8|year=2008|month=July|pmid=18715303|doi=10.1111/j.1445-5994.2008.01715.x|url=http://www3.interscience.wiley.com/resolve/openurl?genre=article&sid=nlm:pubmed&issn=1444-0903&date=2008&volume=38&issue=7&spage=592}}</ref> |
|||
===Other systems=== |
|||
====Respiratory system==== |
|||
Chronic alcohol ingestion can impair multiple critical cellular functions in the lung.{{citation needed|date=January 2013}} These cellular impairments can lead to increased susceptibility to serious complications from lung disease. Recent research cites [[alcoholic lung disease]] as comparable to liver disease in alcohol-related mortality.{{citation needed|date=January 2013}} Alcoholics have a higher risk of developing [[acute respiratory distress syndrome]] (ARDS) and experience higher rates of mortality from ARDS when compared to non-alcoholics.{{citation needed|date=January 2013}} Despite these effects, a large prospective study has shown a protective effect of moderate alcohol consumption on respiratory mortality.<ref name="Doll R, Peto R, Boreham J, Sutherland I 2005 199–204"/> |
|||
====Kidney stones==== |
|||
Research indicates that drinking alcohol is associated with a lower risk of developing [[kidney stones]]. One study concludes, "Since beer seemed to be protective against kidney stones, the physiologic effects of other substances besides ethanol, especially those of hops, should also be examined."<ref>{{cite journal|author=Hirvonen T, Pietinen P, Virtanen M, Albanes D, Virtamo J|title=Nutrient intake and use of beverages and the risk of kidney stones among male smokers|journal=Am J Epidemiol.|volume=150|issue=2|pages=187–94|date=15 July 1999|pmid=10412964|url=http://aje.oxfordjournals.org/cgi/reprint/150/2/187}}</ref> "...consumption of coffee, alcohol, and vitamin C supplements were negatively associated with stones."<ref>{{cite journal|author=Soucie JM, Coates RJ, McClellan W, Austin H, Thun M|title=Relation between geographic variability in kidney stones prevalence and risk factors for stones|journal=Am J Epidemiol.|volume=143|issue=5|pages=487–95|date=1 March 1996|pmid=8610664|url=http://aje.oxfordjournals.org/cgi/reprint/143/5/487}}</ref> "After mutually adjusting for the intake of other beverages, the risk of stone formation decreased by the following amount for each 240-ml (8-oz) serving consumed daily: caffeinated coffee, 10%; decaffeinated coffee, 10%; tea, 14%; beer, 21%; and wine, 39%."<ref>{{cite journal|author=Curhan GC, Willett WC, Rimm EB, Spiegelman D, Stampfer MJ|title=Prospective study of beverage use and the risk of kidney stones|journal=Am J Epidemiol.|volume=143|issue=3|pages=240–7|date=1 February 1996|pmid=8561157|url=http://aje.oxfordjournals.org/cgi/pmidlookup?view=long&pmid=8561157}}</ref> "...stone formation decreased by the following amount for each 240-mL (8-oz) serving consumed daily: 10% for caffeinated coffee, 9% for decaffeinated coffee, 8% for tea, and 59% for wine." ([[Confidence interval|CI]] data excised from last two quotes.).<ref>{{cite journal|author=Curhan GC, Willett WC, Speizer FE, Stampfer MJ|title=Beverage use and risk for kidney stones in women|journal=Ann Intern Med.|volume=128|issue=7|pages=534–40|date=1 April 1998|pmid=9518397|url=http://www.annals.org/cgi/pmidlookup?view=long&pmid=9518397 }}</ref> |
|||
====Sexual dysfunction==== |
|||
Long term excessive intake of alcohol can lead to damage to the [[central nervous system]] and the [[peripheral nervous system]] resulting in loss of sexual desire and impotence in men.<ref>{{cite journal|author=Taniguchi N, Kaneko S|title=[Alcoholic effect on male sexual function]|language=Japanese|journal=Nippon Rinsho|volume=55|issue=11|pages=3040–4|year=1997|month=November|pmid=9396310}}</ref> This can result due to a reduction of testosterone from ethanol-induced [[testicular atrophy]], resulting in increased [[feminisation]] of males and is a clinical feature of alcohol abusing males who have [[cirrhosis]] of the liver.<ref name="pmid9396303">{{cite journal|author=Yoshitsugu M, Ihori M|title=[Endocrine disturbances in liver cirrhosis--focused on sex hormones]|language=Japanese|journal=Nippon Rinsho|volume=55|issue=11|pages=3002–6|year=1997|month=November|pmid=9396303}}</ref> |
|||
====Hormonal Imbalance==== |
|||
Excessive alcohol intake can result in [[hyperoestrogenisation]].<ref>{{Cite journal|last1=Fentiman|first1=IS.|last2=Fourquet|first2=A.|last3=Hortobagyi|first3=GN.|title=Male breast cancer|journal=Lancet|volume=367|issue=9510|pages=595–604|month=Feb|year=2006|doi=10.1016/S0140-6736(06)68226-3|pmid=16488803}}</ref> It has been speculated that alcohol beverages may contain [[estrogen]] like compounds. In men, high levels of estrogen can lead to [[testicular]] failure and the development of feminine traits including development of male breasts, called [[gynecomastia]].<ref>{{Cite journal|last1=Gavaler|first1=JS.|title=Alcoholic beverages as a source of estrogens.|journal=Alcohol Health Res World|volume=22|issue=3|pages=220–7|year=1998|pmid=15706799}}</ref><ref name="Weiss-2005">{{Cite journal|last1=Weiss|first1=JR.|last2=Moysich|first2=KB.|last3=Swede|first3=H.|title=Epidemiology of male breast cancer|journal=Cancer Epidemiol Bio-markers Prev|volume=14|issue=1|pages=20–6|month=Jan|year=2005|url=http://cebp.aacrjournals.org/content/14/1/20.long|pmid=15668471}}</ref> In women, increased levels of estrogen due to excessive alcohol intake have been related to an increased risk of [[breast cancer]].<ref name="Weiss-2005"/><ref>{{Cite journal|last1=Boffetta|first1=P.|last2=Hashibe|first2=M.|title=Alcohol and cancer|journal=Lancet Oncol|volume=7|issue=2|pages=149–56|month=Feb|year=2006|doi=10.1016/S1470-2045(06)70577-0|pmid=16455479}}</ref> |
|||
====Diabetes mellitus==== |
|||
A twenty year twin study from Finland has shown that moderate alcohol consumption may reduce the risk of type 2 diabetes in men and women. However, binge drinking and high alcohol consumption was found to increase the risk of type 2 diabetes in women. |
|||
<ref>{{cite journal|author=Carlsson S, Hammar N, Grill V, Kaprio J|title=Alcohol consumption and the incidence of type 2 diabetes: a 20-year follow-up of the Finnish twin cohort study|journal=Diabetes Care|volume=26|issue=10|pages=2785–90|year=2003|month=October|pmid=14514580|url=http://care.diabetesjournals.org/cgi/content/full/26/10/2785|doi=10.2337/diacare.26.10.2785}}</ref> A study in mice has suggested a beneficial effect of alcohol in promoting [[insulin sensitivity]].<ref>J Hong1, R R Smith, A E Harvey and N P Núñez [http://www.nature.com/ijo/journal/v33/n2/abs/ijo2008266a.html Alcohol consumption promotes insulin sensitivity without affecting body fat levels] ''International Journal of Obesity'' (2009) 33, 197–203; {{doi|10.1038/ijo.2008.266}}</ref> |
|||
====Rheumatoid arthritis==== |
|||
Regular consumption of alcohol is associated with an increased risk of [[gouty arthritis]]<ref>{{cite journal|author=Star VL, Hochberg MC|title=Prevention and management of gout|journal=Drugs|volume=45|issue=2|pages=212–22|year=1993|month=February|pmid=7681372|doi=10.2165/00003495-199345020-00004}}</ref><ref>{{cite journal|author=Eggebeen AT|title=Gout: an update|journal=Am Fam Physician|volume=76|issue=6|pages=801–8|year=2007|month=September|pmid=17910294}}</ref> and a decreased risk of [[rheumatoid arthritis]].<ref>http://arc.org.uk/arthinfo/patpubs/6033/6033.asp</ref><ref>{{cite journal|author=Myllykangas-Luosujärvi R, Aho K, Kautiainen H, Hakala M|title=Reduced incidence of alcohol related deaths in subjects with rheumatoid arthritis|journal=Ann Rheum Dis.|volume=59|issue=1|pages=75–6|year=2000|month=January|pmid=10627433|pmc=1752983|url=http://ard.bmj.com/cgi/pmidlookup?view=long&pmid=10627433|doi=10.1136/ard.59.1.75}}</ref><ref>{{cite journal|author=Nagata C, Fujita S, Iwata H, ''et al.''|title=Systemic lupus erythematosus: a case-control epidemiologic study in Japan|journal=Int J Dermatol.|volume=34|issue=5|pages=333–7|year=1995|month=May|pmid=7607794|doi=10.1111/j.1365-4362.1995.tb03614.x}}</ref><ref>{{cite journal|author=Aho K, Heliövaara M|title=Alcohol, androgens and arthritis|journal=Ann Rheum Dis.|volume=52|issue=12|pages=897|year=1993|month=December|pmid=8311545|pmc=1005228|doi=10.1136/ard.52.12.897-b}}</ref><ref>{{cite journal|author=Hardy CJ, Palmer BP, Muir KR, Sutton AJ, Powell RJ|title=Smoking history, alcohol consumption, and systemic lupus erythematosus: a case-control study|journal=Ann Rheum Dis.|volume=57|issue=8|pages=451–5|year=1998|month=August|pmid=9797548|pmc=1752721|url=http://ard.bmj.com/cgi/content/abstract/57/8/451|doi=10.1136/ard.57.8.451}}</ref> Two recent studies report that the more alcohol consumed, the lower the risk of developing rheumatoid arthritis. Among those who drank regularly, the one-quarter who drank the most were up to 50% less likely to develop the disease compared to the half who drank the least.<ref>{{cite journal|author=Källberg H, Jacobsen S, Bengtsson C, ''et al.''|title=Alcohol consumption is associated with decreased risk of rheumatoid arthritis; Results from two Scandinavian case-control studies|journal=Ann Rheum Dis.|year=2008|month=July|pmid=18535114|pmc=2937278|doi=10.1136/ard.2007.086314|volume=68|pages=222–7|issue=2}}</ref> |
|||
The researchers noted that moderate alcohol consumption also reduces the risk of other inflammatory processes such as cardiovascualar disease. Some of the biological mechanisms by which ethanol reduces the risk of destructive arthritis and prevents the loss of bone mineral density (BMD), which is part of the disease process.<ref>{{cite journal|author=Jonsson IM, Verdrengh M, Brisslert M, ''et al.''|title=Ethanol prevents development of destructive arthritis|journal=Proc Natl Acad Sci USA.|volume=104|issue=1|pages=258–63|year=2007|month=January|pmid=17185416|pmc=1765445|doi=10.1073/pnas.0608620104}}</ref> |
|||
A study concluded, "Alcohol either protects from RA or, subjects with RA curtail their drinking after the manifestation of RA".<ref>{{cite journal|author=Myllykangas-Luosujärvi R, Aho K, Kautiainen H, Hakala M|title=Reduced incidence of alcohol related deaths in subjects with rheumatoid arthritis|journal=Ann Rheum Dis.|volume=59|issue=1|pages=75–6|year=2000|month=January|pmid=10627433|pmc=1752983|url=http://ard.bmj.com/cgi/content/abstract/59/1/75|doi=10.1136/ard.59.1.75}}</ref> Another study found, "Postmenopausal women who averaged more than 14 alcoholic drinks per week had a reduced risk of rheumatoid arthritis..."<ref>{{cite journal|author=Voigt LF, Koepsell TD, Nelson JL, Dugowson CE, Daling JR|title=Smoking, obesity, alcohol consumption, and the risk of rheumatoid arthritis|journal=Epidemiology|volume=5|issue=5|pages=525–32|year=1994|month=September|pmid=7986867}}</ref> |
|||
====Osteoporosis==== |
|||
Moderate alcohol consumption is associated with higher [[bone mineral density]] in postmenopausal women. "...Alcohol consumption significantly decreased the likelihood [of [[osteoporosis]]]."<ref>{{cite journal|author=Siris ES, Miller PD, Barrett-Connor E, ''et al.''|title=Identification and fracture outcomes of undiagnosed low bone mineral density in postmenopausal women: results from the National Osteoporosis Risk Assessment|journal=JAMA|volume=286|issue=22|pages=2815–22|year=2001|month=December|pmid=11735756|url=http://jama.ama-assn.org/cgi/pmidlookup?view=long&pmid=11735756|doi=10.1001/jama.286.22.2815}}</ref> "Moderate alcohol intake was associated with higher BMD in postmenopausal elderly women."<ref>{{cite journal|author=Rapuri PB, Gallagher JC, Balhorn KE, Ryschon KL|title=Alcohol intake and bone metabolism in elderly women|journal=Am. J. Clin. Nutr.|volume=72|issue=5|pages=1206–13|date=1 November 2000|pmid=11063451|url=http://intl.ajcn.org/cgi/content/abstract/72/5/1206}}</ref> "Social drinking is associated with higher bone mineral density in men and women [over 45]."<ref>{{cite journal|author=Holbrook TL, Barrett-Connor E|title=A prospective study of alcohol consumption and bone mineral density|journal=BMJ|volume=306|issue=6891|pages=1506–9|year=1993|month=June|pmid=8518677|pmc=1677960|doi=10.1136/bmj.306.6891.1506}}</ref> However, alcohol abuse is associated with bone loss.<ref name="Ronis-2007">{{Cite journal|last1=Ronis|first1=MJ.|last2=Wands|first2=JR.|last3=Badger|first3=TM.|last4=de la Monte|first4=SM.|last5=Lang|first5=CH.|last6=Calissendorff|first6=J.|title=Alcohol-induced disruption of endocrine signaling.|journal=Alcohol Clin Exp Res|volume=31|issue=8|pages=1269–85|month=Aug|year=2007|doi=10.1111/j.1530-0277.2007.00436.x|pmid=17559547}}</ref><ref name="Peer-">{{Cite journal|last1=Peer|first1=KS.|last2=Newsham|first2=KR.|title=A case study on osteoporosis in a male athlete: looking beyond the usual suspects.|journal=Orthop Nurs|volume=24|issue=3|pages=193–9; quiz 200–1|year=2005|pmid=15928528}}</ref> |
|||
====Skin==== |
|||
Chronic excessive alcohol abuse is associated with a wide range of skin disorders including [[urticaria]], [[porphyria cutanea tarda]], [[flushing (physiology)|flushing]], cutaneous stigmata of [[cirrhosis]], [[psoriasis]], [[pruritus]], [[seborrheic dermatitis]] and [[rosacea]].<ref>{{cite journal|author=Kostović K, Lipozencić J|title=Skin diseases in alcoholics|journal=Acta Dermatovenerol Croat|volume=12|issue=3|pages=181–90|year=2004|pmid=15369644}}</ref> |
|||
A 2010 study concluded, "Nonlight beer intake is associated with an increased risk of developing psoriasis among women. Other alcoholic beverages did not increase the risk of psoriasis in this study."<ref>Abrar A. Qureshi; Patrick L. Dominguez; Hyon K. Choi; Jiali Han; Gary Curhan [http://archderm.ama-assn.org/cgi/content/full/archdermatol.2010.204 Alcohol Intake and Risk of Incident Psoriasis in US Women: A Prospective Study] ''Arch Dermatology'' {{doi|10.1001/archdermatol.2010.204}}</ref> |
|||
===Immune system=== |
|||
====Bacterial infection==== |
|||
There is a protective effect of alcohol consumption against active infection with ''H. pylori''<ref>{{cite journal|author=Brenner H, Rothenbacher D, Bode G, Adler G|title=Relation of smoking and alcohol and coffee consumption to active ''Helicobacter pylori'' infection: cross sectional study|journal=BMJ|volume=315|issue=7121|pages=1489–92|date=6 December 1997|pmid=9420488|pmc=2127930|url=http://bmj.bmjjournals.com/cgi/content/full/315/7121/1489}}</ref> In contrast, alcohol intake (comparing those who drink > 30g of alcohol per day to non-drinkers) is not associated with higher risk of duodenal ulcer.<ref>{{cite journal|author=Aldoori WH, Giovannucci EL, Stampfer MJ, Rimm EB, Wing AL, Willett WC|title=A prospective study of alcohol, smoking, caffeine, and the risk of duodenal ulcer in men|journal=Epidemiology|volume=8|issue=4|pages=420–4|year=1997|month=July|pmid=9209857|url=http://meta.wkhealth.com/pt/pt-core/template-journal/lwwgateway/media/landingpage.htm?issn=1044-3983&volume=8&issue=4&spage=420|doi=10.1097/00001648-199707000-00012}}</ref> Excessive alcohol consumption seen in alcoholics is a known risk factor for pneumonia. |
|||
====Common cold==== |
|||
A study on the common cold found that "Greater numbers of alcoholic drinks (up to three or four per day) were associated with decreased risk for developing colds because drinking was associated with decreased illness following infection. However, the benefits of drinking occurred only among nonsmokers. [...] Although alcohol consumption did not influence risk of clinical illness for smokers, moderate alcohol consumption was associated with decreased risk for nonsmokers."<ref>{{cite journal|author=Cohen S, Tyrrell DA, Russell MA, Jarvis MJ, Smith AP|title=Smoking, alcohol consumption, and susceptibility to the common cold|journal=Am J Public Health|volume=83|issue=9|pages=1277–83|year=1993|month=September|pmid=8363004|pmc=1694990|url=http://www.ajph.org/cgi/reprint/83/9/1277|doi=10.2105/AJPH.83.9.1277}}</ref> |
|||
Another study concluded, "Findings suggest that wine intake, especially red wine, may have a protective effect against common cold. Beer, spirits, and total alcohol intakes do not seem to affect the incidence of common cold."<ref>{{cite journal|author=Takkouche B, Regueira-Méndez C, García-Closas R, Figueiras A, Gestal-Otero JJ, Hernán MA|title=Intake of wine, beer, and spirits and the risk of clinical common cold|journal=Am J Epidemiol.|volume=155|issue=9|pages=853–8|year=2002|month=May|pmid=11978590|url=http://aje.oxfordjournals.org/cgi/content/full/155/9/853|doi=10.1093/aje/155.9.853}}</ref> |
|||
===Cancer=== |
|||
{{Main|Alcohol and cancer}} |
|||
In 1988 the [[International Agency for Research on Cancer]] (Centre International de Recherche sur le Cancer) of the [[World Health Organization]] classified alcohol as a [[List of IARC Group 1 carcinogens|Group 1 carcinogen]], stating "There is sufficient evidence for the carcinogenicity of alcoholic beverages in humans.... Alcoholic beverages are carcinogenic to humans (Group 1)."<ref>IARC Monographs on the Evaluation of Carcinogenic Risks to Humans: Volume 44 ''[http://monographs.iarc.fr/ENG/Monographs/vol44/volume44.pdf Alcohol Drinking: Summary of Data Reported and Evaluation]''</ref> The [[United States Department of Health and Human Services|U.S. Department of Health & Human Services’]] National [[Toxicology]] Program in 2000 listed alcohol as a ''known [[carcinogen]]''.<ref>National Toxicology Program [http://ntp.niehs.nih.gov/ntp/roc/eleventh/profiles/s007alco.pdf Alcoholic Beverage Consumption: Known to be a human carcinogen] First listed in the ''Ninth Report on Carcinogens'' (2000)(PDF)</ref> |
|||
It was estimated in 2006 that "3.6% of all cancer cases worldwide are related to alcohol drinking, resulting in 3.5% of all cancer deaths."<ref name=pmid16557583>{{Cite journal|author=Boffetta P, Hashibe M, La Vecchia C, Zatonski W, Rehm J |title=The burden of cancer attributable to alcohol drinking |journal=International Journal of Cancer |volume=119 |issue=4 |pages=884–7 |year=2006 |month=August |pmid=16557583 |doi=10.1002/ijc.21903}}</ref> A European study from 2011 found that one in 10 of all cancers in men and one in 33 in women were caused by past or current alcohol intake.<ref>BBC [http://www.bbc.co.uk/news/health-12999000 Drinking over recommended limit 'raises cancer risk'] 8 April 2011</ref><ref>Madlen Schütze ''et al'' [http://www.bmj.com/content/342/bmj.d1584.full Alcohol attributable burden of incidence of cancer in eight European countries based on results from prospective cohort study] BMJ 2011; 342:d1584 {{doi|10.1136/bmj.d1584}}</ref> The [[World Cancer Research Fund]] panel report ''Food, Nutrition, Physical Activity and the Prevention of Cancer: a Global Perspective'' finds the evidence "convincing" that alcoholic drinks increase the risk of the following cancers: mouth, pharynx and larynx, oesophagus, colorectum (men), breast (pre- and postmenopause).<ref name=WCRF>WCRF [http://eprints.ucl.ac.uk/4841/1/4841.pdf World Cancer Research Fund / American Institute for Cancer Research. Food, Nutrition, Physical Activity, and the Prevention of Cancer: a Global Perspective. Washington DC: AICR, 2007]</ref> |
|||
[[Acetaldehyde]], a metabolic product of alcohol, is suspected to promote cancer. Typically the liver eliminates 99% of acetaldehyde produced. However, liver disease and certain genetic enzyme deficiencies result in high acetaldehyde levels. Heavy drinkers who are exposed to high acetaldehyde levels due to a genetic defect in [[alcohol dehydrogenase]] have been found to be at greater risk of developing cancers of the upper gastrointestinal tract and liver.<ref>{{cite journal | doi = 10.1002/ijc.21583 | author = Homann N, Stickel F, König IR ''et al.'' | year = 2006| title = Alcohol dehydrogenase 1C*1 allele is a genetic marker for alcohol-associated cancer in heavy drinkers | url = http://www3.interscience.wiley.com/cgi-bin/fulltext/112141765/HTMLSTART | journal = International Journal of Cancer | volume = 118 | issue = 8| pages = 1998–2002 | pmid=16287084}}</ref> A review in 2007 found "convincing evidence that acetaldehyde... is responsible for the carcinogenic effect of ethanol... owing to its multiple mutagenic effects on DNA."<ref>Nat Rev Cancer. 2007 Aug;7(8):599-612. Molecular mechanisms of alcohol-mediated carcinogenesis. Seitz HK, Stickel F. http://www.josorge.com/publications/Citations/JGH/001.pdf</ref> |
|||
Acetaldehyde can react with DNA to create DNA adducts including the Cr-Pdg adduct. This Cr-PdG adduct "is likely to play a central role in the mechanism of alcoholic beverage related carcinogenesis." <ref>Acetaldehyde-DNA Adducts: Implications for the Molecular Mechanism of Alcohol-Related Carcinogenesis Brooks P, Theruvathu J Cho CH, Purohit V (eds): Alcohol, Tobacco and Cancer. Basel, Karger, 2006, pp 78-94 (DOI: 10.1159/000095017) http://content.karger.com/ProdukteDB/produkte.asp?Doi=95017</ref> Some have pointed out that even moderate levels of alcohol consumption are associated with an increased risk of certain forms of cancer.<ref name="Andréasson-"/> |
|||
===Alcohol's effect on the fetus=== |
|||
{{main|Fetal alcohol syndrome|Fetal Alcohol Spectrum Disorder}} |
|||
[[Fetal alcohol syndrome]] or FAS is a disorder of permanent [[birth defect]]s that occurs in the offspring of women who drink [[alcohol]] during pregnancy. Drinking heavily or during the early stages of prenatal development has been conclusively linked to FAS; moderate consumption is associated with fetal damage.<ref name="Andréasson-">{{Cite journal|last1=Andréasson|first1=S.|last2=Allebeck|first2=P.|title=[Alcohol as medication is no good. More risks than benefits according to a survey of current knowledge]|journal=Lakartidningen|volume=102|issue=9|pages=632–7|date=28 February – 6 March 2005|pmid=15804034}}</ref> Alcohol crosses the [[placental barrier]] and can stunt fetal growth or weight, create distinctive facial stigmata, damaged [[neurons]] and brain structures, and cause other physical, mental, or behavioural problems.<ref>{{cite journal|author=Ulleland CN|title=The offspring of alcoholic mothers|journal=Ann. N. Y. Acad. Sci.|volume=197|pages=167–9|year=1972|month=May|pmid=4504588|doi=10.1111/j.1749-6632.1972.tb28142.x}}</ref> Fetal alcohol exposure is the leading known cause of [[mental retardation]] in the Western world.<ref>{{cite journal|author=Abel EL, Sokol RJ|title=Incidence of foetal alcohol syndrome and economic impact of FAS-related anomalies|journal=Drug Alcohol Depend|volume=19|issue=1|pages=51–70|year=1987|month=January|pmid=3545731|url=http://linkinghub.elsevier.com/retrieve/pii/0376-8716(87)90087-1|doi=10.1016/0376-8716(87)90087-1}}</ref> Alcohol consumption during pregnancy is associated with brain [[insulin]] and insulin-like growth factor resistance.<ref name="Ronis-2007"/> |
|||
===Adverse effects of binge drinking (0.08% BAC or higher)=== |
===Adverse effects of binge drinking (0.08% BAC or higher)=== |
||
Revision as of 13:17, 18 February 2013
Alcohol and health is currently a Drugs good article nominee. Nominated by David Hedlund at 2013-02-18 Anyone who has not contributed significantly to (or nominated) this article may review it according to the good article criteria to decide whether or not to list it as a good article. To start the review process, click start review and save the page. (See here for the good article instructions.)
|
Short-term effects of alcohol consumption include intoxication and dehydration. Long-term effects of alcohol include changes in the metabolism of the liver and brain and alcoholism (addiction to alcohol).
Alcohol intoxication affects the brain, causing slurred speech, clumsiness, and delayed reflexes. Alcohol stimulates insulin production, which speeds up glucose metabolism and can result in low blood sugar, causing irritability and (for diabetics) possible death. Severe alcohol poisoning can be fatal.
A blood alcohol content of 0.45% in test animals results in a median lethal dose of LD50. This means that 0.45% is the concentration of blood alcohol that is fatal in 50% of the test subjects. That is about six times the level of ordinary intoxication (0.08%), but vomiting or unconsciousness may occur much sooner in people who have a low tolerance for alcohol.[1] The high tolerance of chronic heavy drinkers may allow some of them to remain conscious at levels above 0.40%, although serious health dangers are incurred at this level.
Alcohol also limits the production of vasopressin (ADH) from the hypothalamus and the secretion of this hormone from the posterior pituitary gland. This is what causes severe dehydration when large amounts of alcohol are drunk. It also causes a high concentration of water in the urine and vomit and the intense thirst that goes along with a hangover.
Stress, hangovers and oral contraceptive pill may increase the desire for alcohol because these things will lower the level of testosterone and alcohol will acutely elevate it.[2] Tobacco has the same effect of increasing the craving for alcohol.[3]
Alcohol expectations
Alcohol expectations are beliefs and attitudes that people have about the effects they will experience when drinking alcoholic beverages. They are largely beliefs about alcohol's effects on a person’s behaviors, abilities, and emotions. Some people believe that if alcohol expectations can be changed, then alcohol abuse might be reduced.[4]
The phenomenon of alcohol expectations recognizes that intoxication has real physiological consequences that alter a drinker's perception of space and time, reduce psychomotor skills, and disrupt equilibrium.[5] The manner and degree to which alcohol expectations interact with the physiological short-term effects of alcohol, resulting in specific behaviors, is unclear.
A single study found, if a society believes that intoxication leads to sexual behavior, rowdy behavior, or aggression, then people tend to act that way when intoxicated. But if a society believes that intoxication leads to relaxation and tranquil behavior, then it usually leads to those outcomes. Alcohol expectations vary within a society, so these outcomes are not certain.[6]
People tend to conform to social expectations, and some societies expect that drinking alcohol will cause disinhibition. However, in societies in which the people do not expect that alcohol will disinhibit, intoxication seldom leads to disinhibition and bad behavior.[5]
Alcohol expectations can operate in the absence of actual consumption of alcohol. Research in the United States over a period of decades has shown that men tend to become more sexually aroused when they think they have been drinking alcohol, — even when they have not been drinking it. Women report feeling more sexually aroused when they falsely believe the beverages they have been drinking contained alcohol (although one measure of their physiological arousal shows that they became less aroused).[citation needed]
Men tend to become more aggressive in laboratory studies in which they are drinking only tonic water but believe that it contains alcohol. They also become less aggressive when they believe they are drinking only tonic water, but are actually drinking tonic water that contains alcohol.[4]
Alcohol and religion
The current Arabic name for alcohol in The Qur'an, in verse 37:47, uses the word الغول al-ġawl —properly meaning "spirit" or "demon"—with the sense "the thing that gives the wine its headiness."[7] The term ethanol was invented 1838, modeled on German äthyl (Liebig), from Greek aither (see ether) + hyle "stuff.". Ether in late 14c. meant "upper regions of space," from Old French ether and directly from Latin aether "the upper pure, bright air," from Greek aither "upper air; bright, purer air; the sky," from aithein "to burn, shine," from PIE root *aidh- "to burn" (see edifice).[8]
Consumption
Some alcoholic beverages have been invested with religious significance, as in the ancient Greco-Roman religion, such as in the ecstatic rituals of Dionysus (also called Bacchus). Some have postulated that pagan religions actively promoted alcohol and drunkenness as a means of fostering fertility. Alcohol was believed to increase sexual desire and to make it easier to approach another person for sex. For example, Norse paganism considered alcohol to be the sap of Yggdrasil. Drunkenness was an important fertility rite in this religion.
Many Christian denominations use wine in the Eucharist or Communion and permit alcohol in moderation. Other denominations use unfermented grape juice in Communion and either abstain from alcohol by choice or prohibit it outright.
Judaism uses wine on Shabbat for Kiddush as well as in the Passover ceremony, Purim, and other religious ceremonies. The drinking of alcohol is allowed. Some Jewish texts, e.g. the Talmud, encourage moderate drinking on holidays (such as Purim) in order to make the occasion more joyous.
Prohibition
Some religions forbid, discourage, or restrict the drinking of alcoholic beverages for various reasons. These include Islam, Jainism, the Bahá'í Faith, The Church of Jesus Christ of Latter-day Saints, the Seventh-day Adventist Church, the Church of Christ, Scientist, the United Pentecostal Church International, Theravada, most Mahayana schools of Buddhism, some Protestant denominations of Christianity, some sects of Taoism (Five Precepts (Taoism) and Ten Precepts (Taoism)), and Hinduism.
The Pali Canon, the scripture of Theravada Buddhism, depicts refraining from alcohol as essential to moral conduct because alcohol causes a loss of mindfulness. The fifth of the Five Precepts states, "Surā-meraya-majja-pamādaṭṭhānā veramaṇī sikkhāpadaṃ samādiyāmi." The English translation is, "I undertake to refrain from fermented drink that causes heedlessness." Technically this prohibition does not cover drugs other than alcohol. But its purport is not that alcohol is an evil but that the carelessness it produces creates bad karma. Therefore any substance (beyond tea or mild coffee) that affects one's mindfulness is considered to be covered by this prohibition.[citation needed]
Abuse prevention
Alcohol abuse prevention programs
0-1-2-3
The Army at Fort Drum has taken the “0-0-1-3” and exchanged it for the new “0-1-2-3” described in the Prime-For-Life Program, which highlights the ill effects of alcohol abuse as more than just an individual’s “driving while intoxicated.” The Prime-For-Life program identifies alcohol abuse to be a health and impairment problem, leading to adverse legal as well as health outcomes associated with misuse.
The 0-1-2-3 now represents low-risk guidelines:
- 0 – Zero drinks for those driving a vehicle.
- 1 – One drink per hour
- 2 – No more than two drinks per day
- 3 – Not to exceed three drinks on any one day
Recommended maximum intake
Binge drinking is becoming a major problem in the UK. Advice on weekly consumption is avoided in United Kingdom.[9]
Since 1995 the UK government has advised that regular consumption of 3–4 units a day for men, or 2–3 units a day for women, would not pose significant health risks, but that consistently drinking four or more units a day (men), or three or more units a day (women), is not advisable.[10]
Previously (from 1992 until 1995), the advice was that men should drink no more than 21 units per week, and women no more than 14.[11] (The difference between the sexes was due to the typically lower weight and water-to-body-mass ratio of women.) This was changed because a government study showed that many people were in effect "saving up" their units and using them at the end of the week, a phenomenon referred to as binge drinking.[citation needed] The Times reported in October 2007 that these limits had been "plucked out of the air" and had no scientific basis.[12]
Sobriety

Sobriety is the condition of not having any measurable levels, or effects from mood-altering drugs. According to WHO "Lexicon of alcohol and drug terms..." sobriety is continued abstinence from psychoactive drug use.[13] Sobriety is also considered to be the natural state of a human being given at a birth. In a treatment setting, sobriety is the achieved goal of independence from consuming or craving mind-altering substances. As such, sustained abstinence is a prerequisite for sobriety. Early in abstinence, residual effects of mind-altering substances can preclude sobriety. These effects are labeled "PAWS", or "post acute withdrawal syndrome". Someone who abstains, but has a latent desire to resume use, is not considered truly sober. An abstainer may be subconsciously motivated to resume drug use, but for a variety of reasons, abstains (e.g. such as a medical or legal concern precluding use).[14] Sobriety has more specific meanings within specific contexts, such as the culture of Alcoholics Anonymous, other 12 step programs, law enforcement, and some schools of psychology. In some cases, sobriety implies achieving "life balance."[15]
Mortality rate
A report of the United States Centers for Disease Control estimated that medium and high consumption of alcohol led to 75,754 deaths in the U.S. in 2001. Low consumption of alcohol had some beneficial effects, so a net 59,180 deaths were attributed to alcohol.[16]
In the United Kingdom, heavy drinking is blamed for about 33,000 deaths a year.[17]
A study in Sweden found that 29% to 44% of "unnatural" deaths (those not caused by illness) were related to alcohol. The causes of death included murder, suicide, falls, traffic accidents, asphyxia, and intoxication.[18]
A global study found that 3.6% of all cancer cases worldwide are caused by alcohol drinking, resulting in 3.5% of all global cancer deaths.[19] A study in the United Kingdom found that alcohol causes about 6% of cancer deaths in the UK (9,000 deaths per year).[20]
ISCD

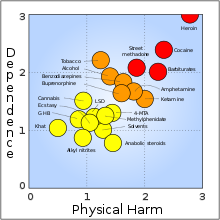
A 2010 study by the Independent Scientific Committee on Drugs, led by David Nutt, Leslie King and Lawrence Phillips, asked drug-harm experts to rank a selection of illegal and legal drugs on various measures of harm both to the user and to others in society. These measures include damage to health, drug dependency, economic costs and crime. The researchers claim that the rankings are stable because they are based on so many different measures and would require significant discoveries about these drugs to affect the rankings.[22]
Despite being legal more often than the other drugs, alcohol was considered to be by far the most harmful; not only was it regarded as the most damaging to societies, it was also seen as the fourth most dangerous for the user. Most of the drugs were rated significantly less harmful than alcohol, with most of the harm befalling the user.
The authors explain that one of the limitation of this study is that drug harms are functions of their availability and legal status in the UK, and so other cultures' control systems could yield different rankings.
Genetic differences
Alcohol flush reaction
Alcohol flush reaction is best known as a condition that is experienced by people of Asian descent. According to the analysis by HapMap project, the rs671 allele of the ALDH2 gene responsible for the flush reaction is rare among Europeans and Africans, and it is very rare among Mexican-Americans. 30% to 50% of people of Chinese and Japanese ancestry have at least one ALDH*2 allele.[23] The rs671 form of ALDH2, which accounts for most incidents of alcohol flush reaction worldwide, is native to East Asia and most common in southeastern China. It most likely originated among Han Chinese in central China,[24] and it appears to have been positively selected in the past. Another analysis correlates the rise and spread of rice cultivation in Southern China with the spread of the allele.[25] The reasons for this positive selection aren't known, but it's been hypothesized that elevated concentrations of acetaldehyde may have conferred protection against certain parasitic infections, such as Entamoeba histolytica.[26]
American Indian alcoholism
While little detailed genetic research has been done, it has been shown that alcoholism tends to run in families with possible involvement of differences in alcohol metabolism and the genotype of alcohol-metabolizing enzymes.
Gender differences
Sensitivity
Several biological factors make women more vulnerable to the effects of alcohol than men.[27]
- Body fat. Women tend to weigh less than men, and—pound for pound—a woman’s body contains less water and more fatty tissue than a man’s. Because fat retains alcohol while water dilutes it, alcohol remains at higher concentrations for longer periods of time in a woman’s body, exposing her brain and other organs to more alcohol.
- Enzymes. Women have lower levels of two enzymes—alcohol dehydrogenase and aldehyde dehydrogenase—that metabolize (break down) alcohol in the stomach and liver. As a result, women absorb more alcohol into their bloodstreams than men.
- Hormones. Changes in hormone levels during the menstrual cycle may also affect how a woman metabolizes alcohol.
Metabolism
Females demonstrated a higher average rate of elimination (mean, 0.017; range, 0.014-0.021 g/210 L) than males (mean, 0.015; range, 0.013-0.017 g/210 L). Female subjects on average had a higher percentage of body fat (mean, 26.0; range, 16.7-36.8%) than males (mean, 18.0; range, 10.2-25.3%).[28]
Depression
The link between alcohol consumption, depression, and gender was examined by the Centre for Addiction and Mental Health (Canada). The study found that women taking antidepressants consumed more alcohol than women who did not experience depression as well as men taking antidepressants. The researchers, Dr. Kathryn Graham and a PhD Student Agnes Massak analyzed the responses to a survey by 14,063 Canadian residents aged 18–76 years. The survey included measures of quantity, frequency of drinking, depression and antidepressants use, over the period of a year. The researchers used data from the GENACIS Canada survey, part of an international collaboration to investigate the influence of cultural variation on gender differences in alcohol use and related problems. The purpose of the study was to examine whether, like in other studies already conducted on male depression and alcohol consumption, depressed women also consumed less alcohol when taking anti-depressants.[29] According to the study, both men and women experiencing depression (but not on anti-depressants) drank more than non-depressed counterparts. Men taking antidepressants consumed significantly less alcohol than depressed men who did not use antidepressants. Non-depressed men consumed 436 drinks per year, compared to 579 drinks for depressed men not using antidepressants, and 414 drinks for depressed men who used antidepressants. Alcohol consumption remained higher whether the depressed women were taking anti-depressants or not. 179 drinks per year for non-depressed women, 235 drinks for depressed women not using antidepressants, and 264 drinks for depressed women who used antidepressants. The lead researcher argued that the study "suggests that the use of antidepressants is associated with lower alcohol consumption among men suffering from depression. But this does not appear to be true for women."[30]
Short-term effects of alcohol
Short-term effects of alcohol on the human body can take many forms. The drug alcohol, to be specific ethanol, is a central nervous system depressant with a range of side-effects. Cell membranes are highly permeable to alcohol, so once alcohol is in the bloodstream it can diffuse into nearly every biological tissue of the body.
The concentration of alcohol in blood is usually measured in terms of the blood alcohol content. The amount and circumstances of consumption play a large part in determining the extent of intoxication; for example, eating a heavy meal before alcohol consumption causes alcohol to absorb more slowly.[31] Hydration also plays a role, especially in determining the extent of hangovers.[32] After excessive drinking, unconsciousness can occur and extreme levels of consumption can lead to alcohol poisoning and death (a concentration in the blood stream of 0.40% will kill half of those affected[33][34]). Alcohol may also cause death by asphyxiation from vomit.
Alcohol is an addictive drug that can greatly exacerbate sleep problems. During abstinence, residual disruptions in sleep regularity and sleep patterns[clarification needed] are the greatest predictors of relapse.[35]
Moderate alcohol consumption and sleep disruptions
Moderate alcohol consumption 30–60 minutes before sleep, although decreasing sleep onset latency, disrupts sleep architecture.[36] Rebound effects occur once the alcohol has been largely metabolized, causing late night disruptions in sleep maintenance. Under conditions of moderate alcohol consumption where blood alcohol levels average 0.06–0.08 percent and decrease 0.01–0.02 percent per hour, an alcohol clearance rate of 4–5 hours would coincide with disruptions in sleep maintenance in the second half of an 8 hour sleep episode.[36] In terms of sleep architecture, moderate doses of alcohol facilitate "rebounds" in rapid eye movement (REM) and stage 1 sleep; following suppression in REM and stage 1 sleep in the first half of an 8 hour sleep episode, REM and stage 1 sleep increase well beyond baseline in the second half. Moderate doses of alcohol also very quickly increase slow wave sleep (SWS) in the first half of an 8 hour sleep episode.[36] Enhancements in REM sleep and SWS following moderate alcohol consumption are mediated by reductions in glutamatergic activity by adenosine in the central nervous system.[36] In addition, tolerance to changes in sleep maintenance and sleep architecture develops within 3 days of alcohol consumption before bedtime.[36]
Alcohol consumption and sleep improvements
Low doses of alcohol (one 360 ml (13 imp fl oz; 12 US fl oz) beer) appear to increase total sleep time and reduce awakening during the night. The sleep-promoting benefits of alcohol dissipate at moderate and higher doses of alcohol.[37] Previous experience with alcohol also influences the extent to which alcohol positively or negatively affects sleep. Under free-choice conditions, in which subjects chose between drinking alcohol or water, inexperienced drinkers were sedated while experienced drinkers were stimulated following alcohol consumption.[38] In insomniacs, moderate doses of alcohol improve sleep maintenance.[39]

Alcohol consumption and fatigue
Conditions of sleep deprivation correlate positively with increased alcohol consumption.[36] In Northern climates, increased alcohol consumption during the winter is attributed to escalations in fatigue.[40]
Alcohol abstinence and sleep disruptions
Hormonal imbalance and sleep disruption following withdrawal from chronic alcohol consumption are strong predictors of relapse.[35] During abstinence, recovering alcoholics have attenuated melatonin secretion at onset of a sleep episode, resulting in prolonged sleep onset latencies.[41] Escalations in cortisol and core body temperatures during the sleep period contribute to poor sleep maintenance.[41][42]
Alcohol consumption and balance
Alcohol affects balance, by changing the viscosity of the endolymph within the otolithic membrane, the fluid inside the semicircular canals inside the ear. The endolymph surrounds the cupula which contains hair cells within the semicircular canals. When the head is tilted, the endolymph flows and moves the cupula. The hair cells then bend and send signals to the brain indicating the direction in which the head is tilted. By changing the viscosity of the endolymph to become less dense when alcohol enters the system, the hair cells can move more easily within the ear, which sends the signal to the brain and results in exaggerated and overcompensated movements of body. This can also result in vertigo, or "the spins."[43][44]
Effects by dosage
Different concentrations of alcohol in the human body have different effects on the subject.
The following lists the common effects of alcohol on the body, depending on the blood alcohol concentration (BAC). However, tolerance varies considerably between individuals, as does individual response to a given dosage; the effects of alcohol differ widely between people. Hence, BAC percentages are just estimates used for illustrative purposes.
|
|
Moderate doses
Ethanol inhibits the ability of glutamate to open the cation channel associated with the N-methyl-D-aspartate (NMDA) subtype of glutamate receptors. Stimulated areas include the cortex, hippocampus and nucleus accumbens, which are responsible for thinking and pleasure seeking. Another one of alcohol's agreeable effects is body relaxation, possibly caused by neurons transmitting electrical signals in an alpha waves-pattern; such waves are observed (with the aid of EEGs) when the body is relaxed.[citation needed]
Short-term effects of alcohol include the risk of injuries, violence and fetal damage.[45] Alcohol has also been linked with lowered inhibitions, though it is unclear to what degree this is chemical versus psychological as studies with placebos can often duplicate the social effects of alcohol at low to moderate doses. Some studies have suggested that intoxicated people have much greater control over their behavior than is generally recognized, though they have a reduced ability to evaluate the consequences of their behavior.[46] Behavioral changes associated with drunkenness are, to some degree, contextual.[47][48] A scientific study[weasel words] found that people drinking in a social setting significantly and dramatically altered their behavior immediately after the first sip of alcohol,[citation needed] well before the chemical itself could have filtered through to the nervous system.
Areas of the brain responsible for planning and motor learning are sharpened. A related effect, caused by even low levels of alcohol, is the tendency for people to become more animated in speech and movement. This is due to increased metabolism in areas of the brain associated with movement, such as the nigrostriatal pathway. This causes reward systems in the brain to become more active, which may induce certain individuals to behave in an uncharacteristically loud and cheerful manner.
Alcohol has been known to mitigate the production of antidiuretic hormone, which is a hormone that acts on the kidney to favour water reabsorption in the kidneys during filtration. This occurs because alcohol confuses osmoreceptors in the hypothalamus, which relay osmotic pressure information to the posterior pituitary, the site of antidiuretic hormone release. Alcohol causes the osmoreceptors to signal that there is low osmotic pressure in the blood, which triggers an inhibition of the antidiuretic hormone. As a consequence, one's kidneys are no longer able to reabsorb as much water as they should be absorbing, leading to creation of excessive volumes of urine and the subsequent overall dehydration.
Excessive doses
Acute alcohol intoxication through excessive doses in general causes short- or long-term health effects. NMDA receptors start to become unresponsive, slowing areas of the brain for which they are responsible. Contributing to this effect is the activity that alcohol induces in the gamma-aminobutyric acid (GABA) system. The GABA system is known to inhibit activity in the brain. GABA could also be responsible for the memory impairment that many people experience. It has been asserted that GABA signals interfere with the registration and consolidation stages of memory formation. As the GABA system is found in the hippocampus (among other areas in the CNS), which is thought to play a large role in memory formation, this is thought to be possible.
Anterograde amnesia, colloquially referred to as "blacking out", is another symptom of heavy drinking. This is the loss of memory during and after an episode of drinking. When alcohol is consumed at a rapid rate, the point at which most healthy people's long-term memory creation starts to fail usually occurs at approximately 0.20% BAC, but can be reached as low as 0.14% BAC for inexperienced drinkers.
Another classic finding of alcohol intoxication is ataxia, in its appendicular, gait, and truncal forms. Appendicular ataxia results in jerky, uncoordinated movements of the limbs, as though each muscle were working independently from the others. Truncal ataxia results in postural instability; gait instability is manifested as a disorderly, wide-based gait with inconsistent foot positioning. Ataxia is responsible for the observation that drunk people are clumsy, sway back and forth, and often fall down. It is presumed to be due to alcohol's effect on the cerebellum.
Pathophysiology

At low or moderate doses, alcohol acts primarily as a positive allosteric modulator of GABAA. Alcohol binds to several different subtypes of GABAA, but not to others. The main subtypes responsible for the subjective effects of alcohol are the α1β3γ2, α5β3γ2, α4β3δ and α6β3δ subtypes, although other subtypes such as α2β3γ2 and α3β3γ2 are also affected. Activation of these receptors causes most of the effects of alcohol such as relaxation and relief from anxiety, sedation, ataxia and increase in appetite and lowering of inhibitions that can cause a tendency toward violence in some people.[49][50][51][52][53][54][55]
Alcohol has a powerful effect on glutamate as well. Alcohol decreases glutamate's ability to bind with NMDA and acts as an antagonist of the NMDA receptor, which plays a critical role in LTP by allowing Ca2+ to enter the cell. These inhibitory effects are thought to be responsible for the "memory blanks" that can occur at levels as low as 0.03% blood level. In addition, reduced glutamate release in the dorsal hippocampus has been linked to spatial memory loss. Chronic alcohol users experience an upregulation of NMDA receptors because the brain is attempting to reestablish homeostasis. When a chronic alcohol user stops drinking for more than 10 hours, apoptosis can occur due to excitotoxicity. The seizures experienced during alcohol abstinence are thought to be a result of this NMDA upregulation. Alteration of NMDA receptor numbers in chronic alcoholics is likely to be responsible for some of the symptoms seen in delirium tremens during severe alcohol withdrawal, such as delirium and hallucinations. Other targets such as sodium channels can also be affected by high doses of alcohol, and alteration in the numbers of these channels in chronic alcoholics is likely to be responsible for as well as other effects such as cardiac arrhythmia. Other targets that are affected by alcohol include cannabinoid, opioid and dopamine receptors, although it is unclear whether alcohol affects these directly or if they are affected by downstream consequences of the GABA/NMDA effects. People with a family history of alcoholism may exhibit genetic differences in the response of their NMDA glutamate receptors as well as the ratios of GABAA subtypes in their brain.[56][57][58][59][60][61][62][63][64][65]
Research
Animal models using mammals and invertebrates have been informative in studying the effects of ethanol on not only pharmacokinetics of alcohol but also pharmacodynamics, in particular in the nervous system. Ethanol-induced intoxication is not uncommon in the animal kingdom, as noted here:
"Many of us have noticed that bees or yellow jackets cannot fly well after having drunk the juice of overripe fruits or berries; bears have been seen to stagger and fall down after eating fermented honey; and birds often crash or fly haphazardly while intoxicated on ethanol that occurs naturally as free-floating microorganisms convert vegetable carbohydrates to alcohol."[66]
More recently, studies using animal models have begun to elucidate the effects of ethanol on the nervous system. Traditionally, many studies have been performed in mammals, such as mice, rats, and non-human primates. However, non-mammalian animal models have also been employed; in particular, Ulrike Heberlein group at UC San Francisco has used Drosophila melanogaster, the fruit fly, taking advantage of its facile genetics to dissect the neural circuits and molecular pathways, upon which ethanol acts. The series of studies carried in the Heberlein lab has identified insulin and its related signaling pathways as well as biogenic amines in the invertebrate nervous system as being important in alcohol tolerance.[67][68][69] The value of antabuse (disulfiram) as a treatment for alcoholism has been tested using another invertebrate animal model, the honey bees.[70] It is important to note that some of the analogous biochemical pathways and neural systems have been known to be important in alcohol's effects on humans, while the possibility that others may also be important remains unknown. Research of alcohol's effects on the nervous system remains a hot topic of research, as scientists inch toward understanding the problem of alcohol addiction.
In addition to the studies carried out in invertebrates, researchers have also used vertebrate animal models to study various effects of ethanol on behaviors.
Blood ethanol concentration (BEC)

BEC chart
The data below apply specifically to ethanol, not other alcohols found in alcoholic beverage.
| Progressive effects of alcohol[71] | ||
|---|---|---|
| BAC (% by vol.) | Behavior | Impairment |
| 0.010–0.029 |
|
|
| 0.030–0.059 |
|
|
| 0.06–0.09 |
|
|
| 0.10–0.19 |
|
|
| 0.20–0.29 |
|
|
| 0.30–0.39 |
|
|
| 0.40–0.50 |
|
|
| >0.50 |
| |
| Male Female |
Approximate blood alcohol percentage (by vol.)[72] One drink has 0.5 US fl oz (15 ml) alcohol by volume | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| Drinks | Body weight | ||||||||
| 40 kg | 45 kg | 55 kg | 64 kg | 73 kg | 82 kg | 91 kg | 100 kg | 109 kg | |
| 90 lb | 100 lb | 120 lb | 140 lb | 160 lb | 180 lb | 200 lb | 220 lb | 240 lb | |
| 1 | – 0.05 |
0.04 0.05 |
0.03 0.04 |
0.03 0.03 |
0.02 0.03 |
0.02 0.03 |
0.02 0.02 |
0.02 0.02 |
0.02 0.02 |
| 2 | – 0.10 |
0.08 0.09 |
0.06 0.08 |
0.05 0.07 |
0.05 0.06 |
0.04 0.05 |
0.04 0.05 |
0.03 0.04 |
0.03 0.04 |
| 3 | – 0.15 |
0.11 0.14 |
0.09 0.11 |
0.08 0.10 |
0.07 0.09 |
0.06 0.08 |
0.06 0.07 |
0.05 0.06 |
0.05 0.06 |
| 4 | – 0.20 |
0.15 0.18 |
0.12 0.15 |
0.11 0.13 |
0.09 0.11 |
0.08 0.10 |
0.08 0.09 |
0.07 0.08 |
0.06 0.08 |
| 5 | – 0.25 |
0.19 0.23 |
0.16 0.19 |
0.13 0.16 |
0.12 0.14 |
0.11 0.13 |
0.09 0.11 |
0.09 0.10 |
0.08 0.09 |
| 6 | – 0.30 |
0.23 0.27 |
0.19 0.23 |
0.16 0.19 |
0.14 0.17 |
0.13 0.15 |
0.11 0.14 |
0.10 0.12 |
0.09 0.11 |
| 7 | – 0.35 |
0.26 0.32 |
0.22 0.27 |
0.19 0.23 |
0.16 0.20 |
0.15 0.18 |
0.13 0.16 |
0.12 0.14 |
0.11 0.13 |
| 8 | – 0.40 |
0.30 0.36 |
0.25 0.30 |
0.21 0.26 |
0.19 0.23 |
0.17 0.20 |
0.15 0.18 |
0.14 0.17 |
0.13 0.15 |
| 9 | – 0.45 |
0.34 0.41 |
0.28 0.34 |
0.24 0.29 |
0.21 0.26 |
0.19 0.23 |
0.17 0.20 |
0.15 0.19 |
0.14 0.17 |
| 10 | – 0.51 |
0.38 0.45 |
0.31 0.38 |
0.27 0.32 |
0.23 0.28 |
0.21 0.25 |
0.19 0.23 |
0.17 0.21 |
0.16 0.19 |
| Subtract approximately 0.01 every 40 minutes after drinking. | |||||||||
Binge drinking
In most jurisdictions a measurement such as a blood alcohol content (BAC) in excess of a specific threshold level, such as 0.05% or 0.08% defines the offense. Also, the National Institute on Alcohol Abuse and Alcoholism (NIAAA) define the term "binge drinking" as any time one reaches a peak BAC of 0.08% or higher as opposed to some (arguably) arbitrary number of drinks in an evening.[73]
Pleasure zone
Known as pleasure zone, the positive exceeds the negative effects typically between 0.030–0.059% blood ethanol concentration (BEC), but contrary at higher volumes like binge drinking (0.08% as defined by NIAAA).
| Standard drink chart (U.S.)[74] | |||||
|---|---|---|---|---|---|
| Alcohol | Amount (ml) | Amount (fl oz) | Serving size | Alcohol (% by vol.) | Alcohol |
| 80 proof liquor | 44 | 1.5 | One shot | 40 | 0.6 US fl oz (18 ml) |
| Table wine | 148 | 5 | One glass | 12 | 0.6 US fl oz (18 ml) |
| Beer | 355 | 12 | One can | 5 | 0.6 US fl oz (18 ml) |
Vehicle operation
The number of serious errors committed by pilots dramatically increases at or above concentrations of 0.04% blood alcohol. This is not to say that problems don't occur below this value. Some studies have shown decrements in pilot performance with blood alcohol concentrations as low as the 0.025%.[75] Also, a BEC of ≥0.080 or more is legally intoxicated for driving in MOST states. And, ≤0.050 is considered NOT impaired in most.[76]
Estimated blood ethanol concentration (EBAC)
In order to calculate estimated peak blood alcohol concentration (EBAC) a variation, including drinking period in hours, of the Widmark formula was used. The formula is:[77]
where 0.806 is a constant for body water in the blood (mean 80.6%), SD is the number of standard drinks containing 10 grams of ethanol, 1.2 is a factor in order to convert the amount in grams to Swedish standards set by The Swedish National Institute of Public Health, BW is a body water constant (0.58 for men and 0.49 for women), Wt is body weight (kilogram), MR is the metabolism constant (0.017), DP is the drinking period in hours and 10 converts the result to permillage of alcohol.[77] Regarding metabolism (MR) in the formula; Females demonstrated a higher average rate of elimination (mean, 0.017; range, 0.014-0.021 g/210 L) than males (mean, 0.015; range, 0.013-0.017 g/210 L). Female subjects on average had a higher percentage of body fat (mean, 26.0; range, 16.7-36.8%) than males (mean, 18.0; range, 10.2-25.3%).[78] Additionally, men are, on average, heavier than women but it is not strictly accurate to say that the water content of a person alone is responsible for the dissolution of alcohol within the body, because alcohol does dissolve in fatty tissue as well. When it does, a certain amount of alcohol is temporarily taken out of the blood and briefly stored in the fat. For this reason, most calculations of alcohol to body mass simply use the weight of the individual, and not specifically his water content. Further, studies have shown that women's alcohol metabolism varies from that of men due to such biochemical factors as different levels of alcohol dehydrogenase (the enzyme which breaks down alcohol) and the effects of oral contraceptives.[79] Finally, it is speculated that the bubbles in sparkling wine may speed up alcohol intoxication by helping the alcohol to reach the bloodstream faster. A study conducted at the University of Surrey in the United Kingdom gave subjects equal amounts of flat and sparkling Champagne which contained the same levels of alcohol. After 5 minutes following consumption, the group that had the sparkling wine had 54 milligrams of alcohol in their blood while the group that had the same sparkling wine, only flat, had 39 milligrams.[80]
Examples:
- 80 kg male drinking 3 standard drinks in two hours:
- 70 kg woman drinking 2.5 standard drinks in two hours:
Useful tools:
Long-term effects of alcohol
| Alcohol and health |
|---|


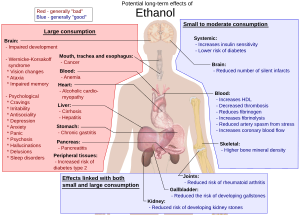
The long term effects of alcohol (ethanol) consumption range from cardioprotective health benefits for low to moderate alcohol consumption in industrialized societies with higher rates of cardiovascular disease[82][83] to severe detrimental effects in cases of chronic alcohol abuse.[84] High levels of alcohol consumption are associated with an increased risk of alcoholism, malnutrition, chronic pancreatitis, alcoholic liver disease, and cancer. In addition damage to the central nervous system and peripheral nervous system can occur from chronic alcohol abuse.[85][86] Long-term use of alcohol in excessive quantities is capable of damaging nearly every organ and system in the body.[87] The developing adolescent brain is particularly vulnerable to the toxic effects of alcohol.[citation needed] In addition, the developing fetal brain is also vulnerable, and fetal alcohol syndrome (FAS) may result if pregnant mothers consume alcohol.[88]
The inverse relation in Western cultures between alcohol consumption and cardiovascular disease has been known for over 100 years.[89] There has been reluctance by many physicians, however, to promote alcohol consumption given the many concerns associated with chronic alcohol abuse. Some even suggest that alcohol should be regarded as a recreational drug, and prefer exercise and good nutrition to combat cardiovascular disease.[90][91] Others have argued that the benefits of moderate alcohol consumption may be outweighed by other increased risks, including those of injuries, violence, fetal damage, liver disease, and certain forms of cancer.[45]
Scientific Studies
Background
The adverse effects of long-term excessive use of alcohol are close to those seen with other sedative-hypnotics (apart from organ toxicity which is much more problematic with alcohol). Withdrawal effects and dependence are also almost identical.[92] Alcohol at moderate levels has some positive and negative effects on health. The negative effects include increased risk of liver diseases, oropharyngeal cancer, esophageal cancer and pancreatitis. Conversely moderate intake of alcohol may have some beneficial effects on gastritis and cholelithiasis.[93] Chronic alcohol misuse and abuse has serious effects on physical and mental health. Chronic excess alcohol intake, or alcohol dependence, can lead to a wide range of neuropsychiatric or neurological impairment, cardiovascular disease, liver disease, and malignant neoplasms. The psychiatric disorders which are associated with alcoholism include major depression, dysthymia, mania, hypomania, panic disorder, phobias, generalized anxiety disorder, personality disorders, schizophrenia, suicide, neurologic deficits (e.g. impairments of working memory, emotions, executive functions, visuospatial abilities and gait and balance) and brain damage. Alcohol dependence is associated with hypertension, coronary heart disease, and ischemic stroke, cancer of the respiratory system, and also cancers of the digestive system, liver, breast and ovaries. Heavy drinking is associated with liver disease, such as cirrhosis.[94] Excessive alcohol consumption can have a negative impact on aging.[95]
Recent studies have focused on understanding the mechanisms by which moderate alcohol consumption confers cardiovascular benefit.[96] One study has suggested a beneficial effect of alcohol on patients with hypertension.[97]
Maximum quantity recommended
Different countries recommend different maximum quantities. For most countries, the maximum quantity for men is 140 g–210 g per week. For women, the range is 84 g–140 g per week.[citation needed] Most countries recommend total abstinence whilst pregnant or breastfeeding.
Over-consumption of alcohol is one of the leading preventable causes of death worldwide.[98] One study links alcohol to 1 in every 25 deaths worldwide and that 5% of years lived with disability are attributable to alcohol consumption.[99][100]
Countries collect statistics on alcohol-related deaths. While some categories relate to short-term effects, such as accidents, many relate to long-term effects of alcohol.
Russia
One study claims that "excessive alcohol consumption in Russia, particularly by men, has in recent years caused more than half of all the deaths at ages 15-54 years."[101] However, there are some difficulties with this study. For instance the same study also found a protective effect of heavy drinking on breast cancer mortality. This contradicts the well established scientific view that alcohol increases breast cancer risk.[102] On this account in further correspondence it was advised that "careful interpretation of mortality statistics in relation to alcohol use is needed, taking into account other relevant risk factors, incidence, and survival."[103]
The authors replied that "whether or not the apparent shortfall in breast cancer mortality among heavy drinkers is real, it accounts for only about 0·1% of adult deaths in Russia. Careful interpretation of it is therefore of little relevance to the findings for alcohol and overall mortality".
United Kingdom
Alcohol-related deaths in the United Kingdom are coded using the Tenth Revision of the International Classification of Diseases (ICD-10).[104] ICD-10 comprises:
- Mental and behavioural disorders due to use of alcohol – ICD-10 F10
- Degeneration of nervous system due to alcohol – ICD-10 G31.2
- Alcoholic polyneuropathy – ICD-10 G62.1
- Alcoholic cardiomyopathy – ICD-10 I42.6
- Alcoholic gastritis – ICD-10 K29.2
- Alcoholic liver disease – ICD-10 K70
- Chronic hepatitis, not elsewhere classified – ICD-10 K73
- Fibrosis and cirrhosis of liver – ICD-10 K74 (Excluding K74.3-K74.5 – Biliary cirrhosis)
- Alcohol induced chronic pancreatitis – ICD-10 K86.0
- Accidental poisoning by and exposure to alcohol – ICD-10 X45
- Intentional self-poisoning by and exposure to alcohol – ICD-10 X65
- Poisoning by and exposure to alcohol, undetermined intent – ICD-10 Y15
UK statistical bodies report that "There were 8,724 alcohol-related deaths in 2007, lower than 2006, but more than double the 4,144 recorded in 1991. The alcohol-related death rate was 13.3 per 100,000 population in 2007, compared with 6.9 per 100,000 population in 1991."[105]
In Scotland, the NHS estimate that in 2003 one in every 20 deaths could be attributed to alcohol.[106]
A 2009 study found that 9,000 people are dying from alcohol-related diseases every year, three times the number 25 years previously.[107]
United States
The Centers for Disease Control and Prevention report, "From 2001–2005, there were approximately 79,000 deaths annually attributable to excessive alcohol use. In fact, excessive alcohol use is the 3rd leading lifestyle-related cause of death for people in the United States each year."[108] A 1993 study estimated US deaths through alcohol at 100,000.[109]
Overall mortality
Extensive research of Western cultures has consistently shown increased survival associated with light to moderate alcohol consumption.[110] A 23-year prospective study of 12,000 male British physicians aged 48–78, found that overall mortality was significantly lower in current drinkers compared to non-drinkers even after correction for ex-drinkers. This benefit was strongest for ischemic heart disease, but was also noted for other vascular disease and respiratory disease. Death rate amongst current drinkers was higher for 'alcohol augmentable' disease such as liver disease and oral cancers, but these deaths were much less common than cardiovascular and respiratory deaths. The lowest mortality rate was found for consumption of 8 to 14 'units' per week. In the UK a unit is defined as 10ml or 8g of pure alcohol.[111] Higher consumption increased overall mortality rate, but not above that of non-drinkers.[112]
This is consistent with other research that found a J-curve dependency between alcohol consumption and total mortality among middle aged and older men. While the mortality rates of ex-drinkers and heavy drinkers are significantly elevated, the all-cause mortality rates may be 15-18% lower among moderate drinkers. Although the definition of a drink varies between studies and countries, this meta-analysis found that low levels of alcohol intake, defined as 1-2 drinks per day for women and 2-4 drinks per day for men, was associated with lower mortality than abstainers.[113] This claim was challenged by another study[114][115] that found that in certain low quality studies occasional drinkers or ex-drinkers were included as abstainers, resulting in the increased mortality in that group. However, the J-curve for total and CHD mortality was reconfirmed by studies that took the mentioned confounders into account.[116][117][118][119]
It has been suggested that the observed decrease in mortality of light-to-moderate drinkers compared to never drinkers might be partially explained by superior health and social status of the drinking group;[120] however, the protective effect of alcohol in light to moderate drinkers remains significant even after adjusting for these confounders.[117][119] Additionally, confounders such as underreporting of alcohol intake might lead to the underestimation of how much mortality is reduced in light-to-moderate drinkers.[116][121]
A 2010 study confirmed the beneficial effect of moderate alcohol consumption on mortality.[119] Subjects were grouped into abstainers, light, moderate, and heavy drinkers. The order of mortality rates from lowest to highest were moderate, light, heavy, and abstainers. The increased risk for abstainers was twice the mortality rate as for moderate drinkers. This study specifically sought to control for confounding factors including the problem of ex-drinkers considered as non-drinkers.[119] According to another study, drinkers with heavy drinking occasions (six or more drinks at a time) have a 57% higher all-cause mortality than drinkers without heavy drinking occasions.[122]
In contrast to studies of Western cultures, research in other cultures has yielded some opposite findings. The landmark INTERHEART Study has revealed that alcohol consumption in South Asians was not protective against CAD in sharp contrast to other populations who benefit from it.[123] In fact Asian Indians who consume alcohol had a 60% higher risk of heart attack which was greater with local spirits (80%) than branded spirits (50%).[124] The harm was observed in alcohol users classified as occasional as well as regular light, moderate, and heavy consumers.[124]
Another large study of 4465 subjects in India also confirmed the possible harm of alcohol consumption on coronary risk in men. Compared to lifetime abstainers, alcohol users had higher blood sugar (2 mg/dl), blood pressure (2 mm Hg) levels, and the HDL-C levels (2 mg/dl) and significantly higher tobacco use (63% vs. 21%).[124]
Cardiovascular system
A meta-analysis of 34 studies found a reduced risk of mortality from coronary heart disease in men who drank 2 - 4 drinks per day and women who drank 1 - 2 drinks per day.[113] Alcohol has been found to have anticoagulant properties.[125][126] Thrombosis is lower among moderate drinkers than abstainers.[127] A meta-analysis of randomized trials found that alcohol consumption in moderation decreases serum levels of fibrinogen, a protein that promotes clot formation, while it increases levels of tissue type plasminogen activator, an enzyme that helps dissolve clots.[128] These changes were estimated to reduce coronary heart disese risk by about 24%.
Serum levels of C-reactive protein (CRP), a marker of inflammation and predictor of CHD (coronary heart disease) risk, are lower in moderate drinkers than in those who abstain from alcohol, suggesting that alcohol consumption in moderation might have anti-inflammatory effects.[129][130][131]
Despite epidemiological evidence, many have cautioned against recommendations for the use of alcohol for health benefits. A physician from the World Health Organisation labeled such alcohol promotion as "ridiculous and dangerous".[132][133] One reviewer has noted, "Despite the wealth of observational data, it is not absolutely clear that alcohol reduces cardiovascular risk, because no randomized controlled trials have been performed. Alcohol should never be recommended to patients to reduce cardiovascular risk as a substitute for the well-proven alternatives of appropriate diet, exercise, and drugs."[134] It has been argued[who?] that the health benefits from alcohol are at best debatable and may have been exaggerated by the alcohol industry. Some investigators hold that alcohol should be regarded as a recreational drug with potentially serious adverse effects on health and should not be promoted for cardio-protection.[90]
Nevertheless, a large prospective non-randomized study has shown that moderate alcohol intake in individuals already at low risk based on body mass index, physical activity, smoking, and diet, yields further improvement in cardiovascular risk.[135]
Peripheral arterial disease
"Moderate alcohol consumption appears to decrease the risk of PAD in apparently healthy men."[136] "In this large population-based study, moderatable alcohol consumption was inversely associated with peripheral arterial disease in women but not in men. Residual confounding by smoking may have influenced the results. Among nonsmokers an inverse association was found between alcohol consumption and peripheral arterial disease in both men and women."[137][138]
Intermittent claudication (IC)
A study found that moderate consumption of alcohol had a protective effect against intermittent claudication. The lowest risk was seen in men who drank 1 to 2 drinks per day and in women who drank half to 1 drink per day.[139]
Heart attack and stroke
Drinking in moderation has been found to help those who have suffered a heart attack survive it.[140][141][142] However, excessive alcohol consumption leads to an increased risk of heart failure.[143] A review of the literature found that half a drink of alcohol offered the best level of protection. However, they noted that at present there have been no randomised trials to confirm the evidence which suggests a protective role of low doses of alcohol against heart attacks.[144] However, moderate alcohol consumption is associated with hypertension.[45] There is an increased risk of hypertriglyceridemia, cardiomyopathy, hypertension, and stroke if 3 or more standard drinks of alcohol are taken per day.[145]
Cardiomyopathy
Large amount of alcohol over the long term can lead to alcoholic cardiomyopathy. Alcoholic cardiomyopathy presents in a manner clinically identical to idiopathic dilated cardiomyopathy, involving hypertrophy of the musculature of the heart that can lead to congestive heart failure.[146]
Hematologic diseases
Alcoholics may have anemia from several causes;[147] they may also develop thrombocytopenia from direct toxic effect on megakaryocytes, or from hypersplenism.
Nervous system

Chronic heavy alcohol consumption impairs brain development, causes brain shrinkage, dementia, physical dependence, increases neuropsychiatric and cognitive disorders and causes distortion of the brain chemistry. Some studies however have shown that moderate alcohol consumption may decrease risk of dementia, including Alzheimer disease, although there are studies which find the opposite. At present, due to poor study design and methodology, the literature is inconclusive on whether moderate alcohol consumption increases the risk of dementia or decreases it.[148] Evidence for a protective effect of low to moderate alcohol consumption on age related cognitive decline and dementia has been suggested by some research, however, other research has not found a protective effect of low to moderate alcohol consumption.[149] Some evidence suggests that low to moderate alcohol consumption may speed up brain volume loss.[150] Chronic consumption of alcohol may result in increased plasma levels of the toxic amino acid homocysteine;[151][152] which may explain alcohol withdrawal seizures,[153] alcohol-induced brain atrophy[154] and alcohol-related cognitive disturbances.[155] Alcohol's impact on the nervous system can also include disruptions of memory and learning (see Effects of alcohol on memory), such as resulting in a blackout phenomenon.
Strokes
Epidemiological studies of middle-aged populations generally find the relationship between alcohol intake and the risk of stroke to be either U- or J-shaped.[156][157][158][159] There may be very different effects of alcohol based on the type of stroke studied. The predominate form of stroke in Western cultures is ischemic, whereas non-western cultures have more hemorrhagic stroke. In contrast to the beneficial effect of alcohol on ischemic stroke, consumption of more than 2 drinks per day increases the risk of hemorrhagic stroke. The National Stroke Association estimates this higher amount of alcohol increases stroke risk by 50%.[160] "For stroke, the observed relationship between alcohol consumption and risk in a given population depends on the proportion of strokes that are hemorrhagic. Light-to-moderate alcohol intake is associated with a lower risk of ischemic stroke which is likely to be, in part, causal. Hemorrhagic stroke, on the other hand, displays a loglinear relationship with alcohol intake."[161]
Brain
Alcohol abuse is associated with widespread and significant brain lesions. Alcohol related brain damage is not only due to the direct toxic effects of alcohol; alcohol withdrawal, nutritional deficiency, electrolyte disturbances, and liver damage are also believed to contribute to alcohol-related brain damage.[162] The long-term effects of alcohol on brain chemistry is an important cause of chronic fatigue.[163]
Adolescent brain development
Consuming large amounts of alcohol over a period of time can impair normal brain development in humans.[164] Deficits in retrieval of verbal and nonverbal information and in visuospatial functioning were evident in youths with histories of heavy drinking during early and middle adolescence.[165][166]
During adolescence critical stages of neurodevelopment occur, including remodeling and functional changes in synaptic plasticity and neuronal connectivity in different brain regions. These changes may make adolescents especially susceptible to the harmful effects of alcohol. Compared to adults, adolescents exposed to alcohol are more likely to exhibit cognitive deficits (including learning and memory dysfunction). Some of these cognitive effects, such as learning impairments, may persist into adulthood.[167]
Mechanisms of action
Neuroinflammation
Ethanol can trigger the activation of astroglial cells which can produce a proinflammatory response in the brain. Ethanol interacts with the TLR4 and IL-1RI receptors on these cells to activate intracellular signal transduction pathways. Specifically, ethanol induces the phosphorylation of IL-1R-associated kinase (IRAK), ERK1/2, stress-activated protein kinase (SAPK)/JNK, and p38 mitogen-activated protein kinase (p38 MAPK). Activation of the IRAK/MAPK pathway leads to the stimulation of the transcription factors NF-kappaB and AP-1. These transcription factors cause the upregulation of inducible nitric oxide synthase (iNOS) and cyclooxygenase-2 (COX-2) expression.[168] The upregulation of these inflammatory mediators by ethanol is also associated with an increase in caspase 3 activity and a corresponding increase in cell apoptosis.[168][169] The exact mechanism by which various concentrations of ethanol either activates or inhibits TLR4/IL-1RI signaling is not currently known, though it may involve alterations in lipid raft clustering [170] or cell adhesion complexes and actin cytoskeleton organization.[171]
Changes in dopaminergic and glutamatergic signaling pathways
Intermittent ethanol treatment causes a decrease in expression of the dopamine receptor type 2 (D2R) and a decrease in phosphorylation of 2B subunit of the NMDA receptor (NMDAR2B) in the prefrontal cortex, hippocampus, nucleus accumbens, and for only D2R the striatum. It also causes changes in the acetylation of histones H3 and H4 in the prefrontal cortex, nucleus accumbens, and striatum, suggesting chromatin remodeling changes which may mediate long-term alterations. Additionally, adolescent rats pre-exposed to ethanol have higher basal levels of dopamine in the nucleus accumbens, along with a prolonged dopamine response in this area in response to a challenge dose of ethanol. Together, these results suggest that alcohol exposure during adolescence can sensitize the mesolimbic and mesocortical dopamine pathways to cause changes in dopaminergic and glutamatergic signaling, which may affect the remodeling and functions of the adolescent brain.[172] These changes are significant as alcohol’s effect on NMDARs could contribute to learning and memory dysfunction (see Effects of alcohol on memory).
Inhibition of hippocampal neurogenesis
Excessive alcohol intake (binge drinking) causes a decrease in hippocampal neurogenesis, via decreases in neural stem cell proliferation and newborn cell survival.[173][174] Alcohol decreases the number of cells in S-phase of the cell cycle, and may arrest cells in the G1 phase, thus inhibiting their proliferation.[173] Ethanol has different effects on different types of actively dividing hippocampal progenitors during their initial phases of neuronal development. Chronic alcohol exposure decreases the number of proliferating cells that are radial glia-like, preneuronal, and intermediate types, while not affecting early neuronal type cells; suggesting ethanol treatment alters the precursor cell pool. Furthermore, there is a greater decrease in differentiation and immature neurons than there is in proliferating progenitors, suggesting that the abnormal decrease in the percentage of actively dividing preneuronal progenitors results in a greater reduction in the maturation and survival of postmitotic cells.[174]
Additionally, alcohol exposure increased several markers of cell death. In these studies neural degeneration seems to be mediated by non-apoptotic pathways.[173][174] One of the proposed mechanisms for alcohol’s neurotoxicity is the production of nitric oxide (NO), yet other studies have found alcohol-induced NO production to lead to apoptosis (see Neuroinflammation section).
Cognition and dementia
Excessive alcohol intake is associated with impaired prospective memory. This impaired cognitive ability leads to increased failure to carry out an intended task at a later date, for example, forgetting to lock the door or to post a letter on time. The higher the volume of alcohol consumed and the longer consumed, the more severe the impairments.[175] One of the organs most sensitive to the toxic effects of chronic alcohol consumption is the brain. In France approximately 20% of admissions to mental health facilities are related to alcohol-related cognitive impairment, most notably alcohol-related dementia. Chronic excessive alcohol intake is also associated with serious cognitive decline and a range of neuropsychiatric complications. The elderly are the most sensitive to the toxic effects of alcohol on the brain.[176] There is some inconclusive evidence that small amounts of alcohol taken in earlier adult life is protective in later life against cognitive decline and dementia.[177] However, a study concluded, "Our findings suggest that, despite previous suggestions, moderate alcohol consumption does not protect older people from cognitive decline."[178]
Acetaldehyde is produced from ethanol metabolism by the liver. The acetaldehyde is further metabolized by the enzyme acetaldehyde dehydrognease. A deficency of this enzyme is not uncommon in individuals from Northeastern Asia as pointed out in a study from Japan.[179] This study has suggested these individuals may be more susceptible to late-onset Alzheimer's disease, however this higher risk is associated with the enzyme deficiency not with alcohol consumption. Individuals with this defect generally do not drink alcohol.
Wernicke-Korsakoff syndrome is a manifestation of thiamine deficiency, usually as a secondary effect of alcohol abuse.[180] The syndrome is a combined manifestation of two eponymous disorders, Korsakoff's Psychosis and Wernicke's encephalopathy, named after Drs. Sergei Korsakoff and Carl Wernicke. Wernicke's encephalopathy is the acute presentation of the syndrome and is characterised by a confusional state while Korsakoff's psychosis main symptoms are amnesia and executive dysfunction.[181]
Essential tremor
Essential tremors can be temporarily relieved in up to two-thirds of patients by drinking small amounts of alcohol.[182]
Ethanol is known to activate aminobutyric acid type A (GABAA) and inhibit N-methyl-D-aspartate (NMDA) glutamate receptors, which are both implicated in essential tremor pathology [183] and could underlie the ameliorative effects.[184][185] Additionally, the effects of ethanol have been studied in different animal essential tremor models.
For more details on this topic, see Essential tremor
Sleep
Chronic use of alcohol used to induce sleep can lead to insomnia. Frequent moving between sleep stages occurs, with awakenings due to headaches and diaphoresis. Stopping chronic alcohol abuse can also lead to profound disturbances of sleep with vivid dreams. Chronic alcohol abuse is associated with NREM stage 3 and 4 sleep as well as suppression of REM sleep and REM sleep fragmentation. During withdrawal REM sleep is typically exaggerated as part of a rebound effect.[186]
Mental health effects
High rates of major depressive disorder occur in heavy drinkers and those who abuse alcohol. Whether it is more true that major depressive disorder causes self-medicating alcohol abuse, or the increased incidence of the disorder in alcohol abusers is caused by the drinking, is not known though some evidence suggests drinking causes the disorder.[187] Alcohol misuse is associated with a number of mental health disorders and alcoholics have a very high suicide rate.[188] A study of people hospitalised for suicide attempts found that those who were alcoholics were 75 times more likely to go on to successfully commit suicide than non-alcoholic suicide attempters.[189] In the general alcoholic population the increased risk of suicide compared to the general public is 5-20 times greater. About 15 percent of alcoholics commit suicide. Abuse of other drugs is also associated with an increased risk of suicide. About 33 percent of suicides in the under 35s are due to alcohol or other substance misuse.[190]
Social skills are significantly impaired in people suffering from alcoholism due to the neurotoxic effects of alcohol on the brain, especially the prefrontal cortex area of the brain. The social skills that are impaired by alcohol abuse include impairments in perceiving facial emotions, prosody perception problems and theory of mind deficits; the ability to understand humour is also impaired in alcohol abusers.[191]
Studies have shown that alcohol dependence relates directly to cravings and irritability.[192] Another study has shown that alcohol use is a significant predisposing factor towards antisocial behavior in children.[193] Depression, anxiety and panic disorder are disorders commonly reported by alcohol dependent people. Alcoholism is associated with dampened activation in brain networks responsible for emotional processing (e.g. the amygdala and hippocampus).[194] Evidence that the mental health disorders are often induced by alcohol misuse via distortion of brain neurochemistry is indicated by the improvement or disappearance of symptoms that occurs after prolonged abstinence, although problems may worsen in early withdrawal and recovery periods.[195][196][197] Psychosis is secondary to several alcohol-related conditions including acute intoxication and withdrawal after significant exposure.[198] Chronic alcohol misuse can cause psychotic type symptoms to develop, more so than with other drugs of abuse. Alcohol abuse has been shown to cause an 800% increased risk of psychotic disorders in men and a 300% increased risk of psychotic disorders in women which are not related to pre-existing psychiatric disorders. This is significantly higher than the increased risk of psychotic disorders seen from cannabis use making alcohol abuse a very significant cause of psychotic disorders.[199] Approximately 3 percent of people who are alcohol dependent experience psychosis during acute intoxication or withdrawal. Alcohol-related psychosis may manifest itself through a kindling mechanism. The mechanism of alcohol-related psychosis is due to distortions to neuronal membranes, gene expression, as well as thiamin deficiency. It is possible in some cases that alcohol abuse via a kindling mechanism can cause the development of a chronic substance-induced psychotic disorder, i.e. schizophrenia. The effects of an alcohol-related psychosis include an increased risk of depression and suicide as well as psychosocial impairments.[198]
While alcohol initially helps social phobia or panic symptoms, with longer term alcohol misuse can often worsen social phobia symptoms and can cause panic disorder to develop or worsen, during alcohol intoxication and especially during the alcohol withdrawal syndrome. This effect is not unique to alcohol but can also occur with long term use of drugs which have a similar mechanism of action to alcohol such as the benzodiazepines which are sometimes prescribed as tranquillisers to people with alcohol problems.[200] Approximately half of patients attending mental health services for conditions including anxiety disorders such as panic disorder or social phobia suffer from alcohol or benzodiazepine dependence. It was noted that every individual has an individual sensitivity level to alcohol or sedative hypnotic drugs and what one person can tolerate without ill health another will suffer very ill health and that even moderate drinking can cause rebound anxiety syndromes and sleep disorders. A person who is suffering the toxic effects of alcohol will not benefit from other therapies or medications as they do not address the root cause of the symptoms.[201]
Digestive system and weight gain
The impact of alcohol on weight-gain is contentious: some studies find no effect,[202] others find decreased[203] or increased effect on weight gain.
Alcohol use increases the risk of chronic gastritis (stomach inflammation);[204][205] it is one cause of cirrhosis, hepatitis, and pancreatitis in both its chronic and acute forms.
Metabolic syndrome
A study concluded, "Mild to moderate alcohol consumption is associated with a lower prevalence of the metabolic syndrome, with a favorable influence on lipids, waist circumference, and fasting insulin. This association was strongest among whites and among beer and wine drinkers."[206] This is also true for Asians. A J-curve association between alcohol intake and metabolic syndrome was found: "The results of the present study suggest that the metabolic syndrome is negatively associated with light alcohol consumption (1–15 g alcohol/d) in Korean adults". However, "odds ratios for the metabolic syndrome and its components tended to increase with increasing alcohol consumption."[207]
Gallbladder effects
Research has found that drinking reduces the risk of developing gallstones. Compared with alcohol abstainers, the relative risk of gallstone disease, controlling for age, sex, education, smoking, and body mass index, is 0.83 for occasional and regular moderate drinkers (< 25 ml of ethanol per day), 0.67 for intermediate drinkers (25-50 ml per day), and 0.58 for heavy drinkers. This inverse association was consistent across strata of age, sex, and body mass index."[208] Frequency of drinking also appears to be a factor. "An increase in frequency of alcohol consumption also was related to decreased risk. Combining the reports of quantity and frequency of alcohol intake, a consumption pattern that reflected frequent intake (5-7 days/week) of any given amount of alcohol was associated with a decreased risk, as compared with nondrinkers. In contrast, infrequent alcohol intake (1-2 days/week) showed no significant association with risk."[209]
Consumption of alcohol is unrelated to gallbladder disease.[210] However one study suggested that drinkers who take vitamin C (ascorbic acid) might reduce their risk of gallbladder disease.[211]
Liver disease
Alcoholic liver disease is a major public health problem. For example in the United States up to two million people have alcohol-related liver disorders.[212] Chronic alcohol abuse can cause fatty liver, cirrhosis and alcoholic hepatitis. Treatment options are limited and consist of most importantly discontinuing alcohol consumption. In cases of severe liver disease, the only treatment option may be a liver transplant in alcohol abstinent patients. Research is being conducted into the effectiveness of anti-TNFs. Certain complementary medications, e.g., milk thistle and silymarin, appear to offer some benefit.[212][213] Alcohol is a leading cause of liver cancer in the Western world, accounting for 32-45% of hepatic cancers. Up to half a million people in the United States develop alcohol-related liver cancer.[214][215] Moderate alcohol consumption also increases the risk of liver disease.[45]
Pancreatitis
Alcohol misuse is a leading cause of both acute pancreatitis and chronic pancreatitis.[216][217] Chronic excessive intake of alcohol can cause destruction of the pancreas resulting in severe chronic pain, which may progress to pancreatic cancer.[218] Chronic pancreatitis often results in malabsorption problems and diabetes.[219]
Other systems
Respiratory system
Chronic alcohol ingestion can impair multiple critical cellular functions in the lung.[citation needed] These cellular impairments can lead to increased susceptibility to serious complications from lung disease. Recent research cites alcoholic lung disease as comparable to liver disease in alcohol-related mortality.[citation needed] Alcoholics have a higher risk of developing acute respiratory distress syndrome (ARDS) and experience higher rates of mortality from ARDS when compared to non-alcoholics.[citation needed] Despite these effects, a large prospective study has shown a protective effect of moderate alcohol consumption on respiratory mortality.[112]
Kidney stones
Research indicates that drinking alcohol is associated with a lower risk of developing kidney stones. One study concludes, "Since beer seemed to be protective against kidney stones, the physiologic effects of other substances besides ethanol, especially those of hops, should also be examined."[220] "...consumption of coffee, alcohol, and vitamin C supplements were negatively associated with stones."[221] "After mutually adjusting for the intake of other beverages, the risk of stone formation decreased by the following amount for each 240-ml (8-oz) serving consumed daily: caffeinated coffee, 10%; decaffeinated coffee, 10%; tea, 14%; beer, 21%; and wine, 39%."[222] "...stone formation decreased by the following amount for each 240-mL (8-oz) serving consumed daily: 10% for caffeinated coffee, 9% for decaffeinated coffee, 8% for tea, and 59% for wine." (CI data excised from last two quotes.).[223]
Sexual dysfunction
Long term excessive intake of alcohol can lead to damage to the central nervous system and the peripheral nervous system resulting in loss of sexual desire and impotence in men.[224] This can result due to a reduction of testosterone from ethanol-induced testicular atrophy, resulting in increased feminisation of males and is a clinical feature of alcohol abusing males who have cirrhosis of the liver.[225]
Hormonal Imbalance
Excessive alcohol intake can result in hyperoestrogenisation.[226] It has been speculated that alcohol beverages may contain estrogen like compounds. In men, high levels of estrogen can lead to testicular failure and the development of feminine traits including development of male breasts, called gynecomastia.[227][228] In women, increased levels of estrogen due to excessive alcohol intake have been related to an increased risk of breast cancer.[228][229]
Diabetes mellitus
A twenty year twin study from Finland has shown that moderate alcohol consumption may reduce the risk of type 2 diabetes in men and women. However, binge drinking and high alcohol consumption was found to increase the risk of type 2 diabetes in women. [230] A study in mice has suggested a beneficial effect of alcohol in promoting insulin sensitivity.[231]
Rheumatoid arthritis
Regular consumption of alcohol is associated with an increased risk of gouty arthritis[232][233] and a decreased risk of rheumatoid arthritis.[234][235][236][237][238] Two recent studies report that the more alcohol consumed, the lower the risk of developing rheumatoid arthritis. Among those who drank regularly, the one-quarter who drank the most were up to 50% less likely to develop the disease compared to the half who drank the least.[239]
The researchers noted that moderate alcohol consumption also reduces the risk of other inflammatory processes such as cardiovascualar disease. Some of the biological mechanisms by which ethanol reduces the risk of destructive arthritis and prevents the loss of bone mineral density (BMD), which is part of the disease process.[240]
A study concluded, "Alcohol either protects from RA or, subjects with RA curtail their drinking after the manifestation of RA".[241] Another study found, "Postmenopausal women who averaged more than 14 alcoholic drinks per week had a reduced risk of rheumatoid arthritis..."[242]
Osteoporosis
Moderate alcohol consumption is associated with higher bone mineral density in postmenopausal women. "...Alcohol consumption significantly decreased the likelihood [of osteoporosis]."[243] "Moderate alcohol intake was associated with higher BMD in postmenopausal elderly women."[244] "Social drinking is associated with higher bone mineral density in men and women [over 45]."[245] However, alcohol abuse is associated with bone loss.[246][247]
Skin
Chronic excessive alcohol abuse is associated with a wide range of skin disorders including urticaria, porphyria cutanea tarda, flushing, cutaneous stigmata of cirrhosis, psoriasis, pruritus, seborrheic dermatitis and rosacea.[248]
A 2010 study concluded, "Nonlight beer intake is associated with an increased risk of developing psoriasis among women. Other alcoholic beverages did not increase the risk of psoriasis in this study."[249]
Immune system
Bacterial infection
There is a protective effect of alcohol consumption against active infection with H. pylori[250] In contrast, alcohol intake (comparing those who drink > 30g of alcohol per day to non-drinkers) is not associated with higher risk of duodenal ulcer.[251] Excessive alcohol consumption seen in alcoholics is a known risk factor for pneumonia.
Common cold
A study on the common cold found that "Greater numbers of alcoholic drinks (up to three or four per day) were associated with decreased risk for developing colds because drinking was associated with decreased illness following infection. However, the benefits of drinking occurred only among nonsmokers. [...] Although alcohol consumption did not influence risk of clinical illness for smokers, moderate alcohol consumption was associated with decreased risk for nonsmokers."[252]
Another study concluded, "Findings suggest that wine intake, especially red wine, may have a protective effect against common cold. Beer, spirits, and total alcohol intakes do not seem to affect the incidence of common cold."[253]
Cancer
In 1988 the International Agency for Research on Cancer (Centre International de Recherche sur le Cancer) of the World Health Organization classified alcohol as a Group 1 carcinogen, stating "There is sufficient evidence for the carcinogenicity of alcoholic beverages in humans.... Alcoholic beverages are carcinogenic to humans (Group 1)."[254] The U.S. Department of Health & Human Services’ National Toxicology Program in 2000 listed alcohol as a known carcinogen.[255]
It was estimated in 2006 that "3.6% of all cancer cases worldwide are related to alcohol drinking, resulting in 3.5% of all cancer deaths."[256] A European study from 2011 found that one in 10 of all cancers in men and one in 33 in women were caused by past or current alcohol intake.[257][258] The World Cancer Research Fund panel report Food, Nutrition, Physical Activity and the Prevention of Cancer: a Global Perspective finds the evidence "convincing" that alcoholic drinks increase the risk of the following cancers: mouth, pharynx and larynx, oesophagus, colorectum (men), breast (pre- and postmenopause).[259]
Acetaldehyde, a metabolic product of alcohol, is suspected to promote cancer. Typically the liver eliminates 99% of acetaldehyde produced. However, liver disease and certain genetic enzyme deficiencies result in high acetaldehyde levels. Heavy drinkers who are exposed to high acetaldehyde levels due to a genetic defect in alcohol dehydrogenase have been found to be at greater risk of developing cancers of the upper gastrointestinal tract and liver.[260] A review in 2007 found "convincing evidence that acetaldehyde... is responsible for the carcinogenic effect of ethanol... owing to its multiple mutagenic effects on DNA."[261]
Acetaldehyde can react with DNA to create DNA adducts including the Cr-Pdg adduct. This Cr-PdG adduct "is likely to play a central role in the mechanism of alcoholic beverage related carcinogenesis." [262] Some have pointed out that even moderate levels of alcohol consumption are associated with an increased risk of certain forms of cancer.[45]
Alcohol's effect on the fetus
Fetal alcohol syndrome or FAS is a disorder of permanent birth defects that occurs in the offspring of women who drink alcohol during pregnancy. Drinking heavily or during the early stages of prenatal development has been conclusively linked to FAS; moderate consumption is associated with fetal damage.[45] Alcohol crosses the placental barrier and can stunt fetal growth or weight, create distinctive facial stigmata, damaged neurons and brain structures, and cause other physical, mental, or behavioural problems.[263] Fetal alcohol exposure is the leading known cause of mental retardation in the Western world.[264] Alcohol consumption during pregnancy is associated with brain insulin and insulin-like growth factor resistance.[246]
Adverse effects of binge drinking (0.08% BAC or higher)
The National Institute on Alcohol Abuse and Alcoholism (NIAAA) recently redefined the term "binge drinking" as any time one reaches a peak BAC of 0.08% or higher as opposed to some (arguably) arbitrary number of drinks in an evening.[73]
Alcohol withdrawal syndrome
The severity of the alcohol withdrawal syndrome can vary from mild symptoms such as mild sleep disturbances and mild anxiety to very severe and life threatening including delirium, particularly visual hallucinations in severe cases and convulsions (which may result in death).[265] This is sometimes referred to as alcohol-induced physical dependency; Sedative hypnotic drugs such as alcohol, benzodiazepines, and barbiturates are the only commonly available substances that can be fatal in withdrawal due to their propensity to induce withdrawal convulsions.
High-functioning alcoholic (HFA)
A high-functioning alcoholic (HFA) is a form of alcoholism where the alcoholic is able to maintain their outside life such as jobs, academics, relationships, etc. – all while drinking alcoholically.[266]
Many HFAs are not viewed by society as alcoholics because they do not fit the common alcoholic stereotype. Unlike the stereotypical alcoholic, HFAs have either succeeded or over-achieved through their lifetimes. This can lead to denial of alcoholism by both the HFA, co-workers, family members and friends. Functional alcoholics account for 19.5 percent of total U.S. alcoholics, with 50 percent being smokers and 33 percent having a multigenerational family history of alcoholism.[267]
Alcoholism
Alcohol is the most available and widely abused substance; Beer alone is the world's most widely consumed[268] alcoholic beverage; it is the third-most popular drink overall, after water and tea.[269] It is thought by some to be the oldest fermented beverage.[270][271][272][273]
Under the DSM's new definition of Alcoholism about 37 percent of college students may meet the criteria. Doctors are hoping that this new definition of the term will help catch severe cases of alcoholism early, instead of when the problem is full-blown.[274]
Based on combined data from SAMHSA's 2004-2005 National Surveys on Drug Use & Health, the rate of past year alcohol dependence or abuse among persons aged 12 or older varied by level of alcohol use: 44.7% of past month heavy drinkers, 18.5% binge drinkers, 3.8% past month non-binge drinkers, and 1.3% of those who did not drink alcohol in the past month met the criteria for alcohol dependence or abuse in the past year. Males had higher rates than females for all measures of drinking in the past month: any alcohol use (57.5% vs. 45%), binge drinking (30.8% vs. 15.1%), and heavy alcohol use (10.5% vs. 3.3%), and males were twice as likely as females to have met the criteria for alcohol dependence or abuse in the past year (10.5% vs. 5.1%).[275]
The National Institute on Alcohol Abuse and Alcoholism defines binge drinking as the amount of alcohol leading to a blood alcohol content (BAC) of 0.08, which, for most adults, would be reached by consuming five drinks for men or four for women over a 2-hour period.
According to the National Institute on Alcohol Abuse and Alcoholism [NIAAA], men may be at risk for alcohol-related problems if their alcohol consumption exceeds 14 standard drinks per week or 4 drinks per day, and women may be at risk if they have more than 7 standard drinks per week or 3 drinks per day. A standard drink is defined as one 12-ounce bottle of beer, one 5-ounce glass of wine, or 1.5 ounces of distilled spirits.)[276]
Alcoholism can lead to malnutrition because it can alter digestion and the metabolism of most nutrients. Severe thiamine deficiency is common in alcoholism due to deficiency of folate, riboflavin, vitamin B6, and selenium ; this can lead to Korsakoff's syndrome. Alcoholism is also associated with a type of dementia called Wernicke-Korsakoff syndrome, which is caused by a deficiency in thiamine (vitamin B1).[277] Muscle cramps, nausea, loss of appetite, nerve disorders, and depression are common symptoms of alcoholism. Osteoporosis and bone fractures may occur due to deficiency of vitamin D.
Cancer
Alcohol consumption has been linked with seven types of cancer: mouth cancer, pharyngeal cancer, oesophageal cancer, laryngeal cancer, breast cancer, bowel cancer and liver cancer.[20] Heavy drinkers are more likely to develop liver cancer due to cirrhosis of the liver.[20] The risk of developing cancer increases even with consumption of as little as three units of alcohol (one pint of lager or a large glass of wine) a day.[20]
A global study found that 3.6% of all cancer cases worldwide are caused by drinking alcohol, resulting in 3.5% of all global cancer deaths.[19] A study in the United Kingdom found that alcohol causes about 6% of cancer deaths in the UK (9,000 deaths per year).[20] A study in China found that alcohol causes about 4.40% of all cancer deaths and 3.63% of all cancer incidences.[278] For both men and women, the consumption of two or more drinks daily increases the risk of pancreatic cancer by 22%.[279]
Women who regularly consume low to moderate amounts of alcohol have an increased risk of cancer of the upper digestive tract, rectum, liver, and breast.[280][281]
Red wine contains resveratrol, which has some anti-cancer effect. However, based on studies done so far, there is no strong evidence that red wine protects against cancer in humans.[282]
Recent studies indicate that Asian populations are particularly prone to carcinogenic effects of alcohol. It's been noted that ethanol's byproducts in metabolism results in acetaldehyde. In non-Asian populations, an enzyme called alcohol dehydrogenase that quickly converts acetaldehyde into acetate. Asian populations have a variant form of alcohol dehydrogenase which prevents conversion of the acetaldehyde. This substance has been indicated to have strong interactions with DNA and thereby causing carcinogenic effects.[283][284]
Dementia
Excessive drinking has been linked to dementia; it is estimated that 10% to 24% of dementia cases are caused by alcohol consumption, with women being at greater risk than men.[285][286]
Alcoholism is associated with a type of dementia called Wernicke–Korsakoff syndrome, which is caused by a deficiency in thiamine (vitamin B1).[277]
In people aged 55 or older, daily light-to-moderate drinking (one to three drinks) was associated with a 42% reduction in the probability of developing dementia and a 70% reduction in risk of vascular dementia.[287] The researchers suggest that alcohol may stimulate the release of acetylcholine in the hippocampus area of the brain.[287]
Diabetes
If both parents have type 2 diabetes, this increases to a 45 percent chance.[288]
Hip fracture
An international study[289] of almost 6,000 men and 11,000 women found that persons who reported that they drank more than 2 units of alcohol a day had an increased risk of fractures compared to non-drinkers. For example, those who drank over 3 units a day had nearly twice the risk of a hip fracture.
Obesity
Biological and environmental factors are thought to contribute to alcoholism and obesity.[290] The physiologic commonalities between excessive eating and excessive alcohol drinking shed light on intervention strategies, such as pharmaceutical compounds that may help those who suffer from both. Some of the brain signaling proteins that mediate excessive eating and weight gain also mediate uncontrolled alcohol consumption.[290] Some physiological substrates that underlie food intake and alcohol intake have been identified. Melanocortins, a group of signaling proteins, are found to be involved in both excessive food intake and alcohol intake.[291]
Alcohol may contribute to obesity. A study found frequent, light drinkers (three to seven drinking days per week, one drink per drinking day) had lower BMIs than infrequent, but heavier drinkers.[292] Although calories in liquids containing ethanol may fail to trigger the physiologic mechanism that produces the feeling of fullness in the short term; long-term, frequent drinkers may compensate for energy derived from ethanol by eating less.[35]
Neurotoxin

As a neurotoxin, ethanol has been shown to induce nervous system damage and affect the body in a variety of ways. Among the known effects of ethanol exposure are both transient and lasting consequences. Some of the lasting effects include long-term reduced neurogenesis in the hippocampus,[293][294] widespread brain atrophy,[295] and induced inflammation in the brain.[296] Of note, chronic ethanol ingestion has additionally been shown to induce reorganization of cellular membrane constituents, leading to a lipid bilayer marked by increased membrane concentrations of cholesterol and saturated fat.[297] This is important as neurotransmitter transport can be impaired through vesicular transport inhibition, resulting in diminished neural network function. One significant example of reduced inter-neuron communication is the ability for ethanol to inhibit NMDA receptors in the hippocampus, resulting in reduced LTP (long-term potentiation) and memory acquisition.[298] NMDA has been shown to play an important role in long-term potentiation (LTP) and consequently memory formation.[299] With chronic ethanol intake, however, the susceptibility of these NMDA receptors to induce LTP increases in the mesolimbic dopamine neurons in an inositol 1,4,5-triphosphate (IP3) dependent manner.[300] This reorganization may lead to neuronal cytotoxicity both through hyperactivation of postsynaptic neurons and through induced addiction to continuous ethanol consumption. It has, additionally, been shown that ethanol directly reduces intracellular calcium ion accumulation through inhibited NMDA receptor activity, and thus reduces the capacity for the occurrence of LTP.[301]
In addition to the neurotoxic effects of ethanol in mature organisms, chronic ingestion is capable of inducing severe developmental defects. Evidence was first shown in 1973 of a connection between chronic ethanol intake by mothers and defects in their offspring.[302] This work was responsible for creating the classification of fetal alcohol syndrome; a disease characterized by common morphogenesis aberrations such as defects in craniofacial formation, limb development, and cardiovascular formation. The magnitude of ethanol neurotoxicity in fetuses leading to fetal alcohol syndrome has been shown to be dependent on antioxidant levels in the brain such as vitamin E.[303] As the fetal brain is relatively fragile and susceptible to induced stresses, severe deleterious effects of alcohol exposure can be seen in important areas such as the hippocampus and cerebellum. The severity of these effects is directly dependent upon the amount and frequency of ethanol consumption by the mother, and the stage in development of the fetus.[304] It is known that ethanol exposure results in reduced antioxidant levels, mitochondrial dysfunction (Chu 2007), and subsequent neuronal death, seemingly as a result of increased generation of reactive oxidative species (ROS).[305] This is a plausible mechanism, as there is a reduced presence in the fetal brain of antioxidant enzymes such as catalase and peroxidase.[306] In support of this mechanism, administration of high levels of dietary vitamin E results in reduced or eliminated ethanol-induced neurotoxic effects in fetuses.[307]
Self-medication
Alcohol and sedative/hypnotic drugs, such as barbiturates and benzodiazepines, are central nervous system (CNS) depressants, which produce feelings of relaxation, and sedation, while relieving feelings of depression and anxiety. Alcohol also lowers inhibitions, while benzodiazepines are anxiolytic. Though they are generally ineffective antidepressants, as most are short-acting, the rapid onset of alcohol and sedative/hypnotics softens rigid defenses and, in low to moderate doses, provides the illusion of relief from depressive affect and anxiety.[1][2] As alcohol also lowers inhibitions, alcohol is also hypothesized to be used by those who normally constrain emotions by attenuating intense emotions in high or obliterating doses, which allows them to express feelings of affection, aggression, and closeness.[8][2]
- Anxiolytics/Antidepressant
Alcohol and sedative/hypnotic drugs, such as barbiturates and benzodiazepines, are central nervous system (CNS) depressants that lower inhibitions via anxiolysis. Depressants produce feelings of relaxation and sedation, while relieving feelings of depression and anxiety. Though they are generally ineffective antidepressants, as most are short-acting, the rapid onset of alcohol and sedative/hypnotics softens rigid defenses and, in low to moderate doses, provides relief from depressive affect and anxiety.[308][309] As alcohol also lowers inhibitions, alcohol is also hypothesized to be used by those who normally constrain emotions by attenuating intense emotions in high or obliterating doses, which allows them to express feelings of affection, aggression and closeness.[309][310] People with social anxiety disorder commonly use these drugs to overcome their highly set inhibitions.[311]
Self medicating excessively for prolonged periods of time with benzodiazepines or alcohol often makes the symptoms of anxiety or depression worse. This is believed to occur as a result of the changes in brain chemistry from long-term use.[312][313][314][315][316] Of those who seek help from mental health services for conditions including anxiety disorders such as panic disorder or social phobia, approximately half have alcohol or benzodiazepine dependence issues.[317]
Sometimes anxiety precedes alcohol or benzodiazepine dependence but the alcohol or benzodiazepine dependence acts to keep the anxiety disorders going, often progressively making them worse. However, some people addicted to alcohol or benzodiazepines, when it is explained to them that they have a choice between ongoing poor mental health or quitting and recovering from their symptoms, decide on quitting alcohol or benzodiazepines or both. It has been noted that every individual has an individual sensitivity level to alcohol or sedative hypnotic drugs, and what one person can tolerate without ill health, may cause another to suffer very ill health, and even moderate drinking can cause rebound anxiety syndrome and sleep disorders. A person suffering the toxic effects of alcohol will not benefit from other therapies or medications, as these do not address the root cause of the symptoms.[317]
- Insomnia
Alcohol is often used as a form of self-treatment of insomnia to induce sleep. However, alcohol use to induce sleep can be a cause of insomnia. Long-term use of alcohol is associated with a decrease in NREM stage 3 and 4 sleep as well as suppression of REM sleep and REM sleep fragmentation. Frequent moving between sleep stages occurs, with awakenings due to headaches, the need to urinate, dehydration, and excessive sweating. Glutamine rebound also plays a role as when someone is drinking; alcohol inhibits glutamine, one of the body's natural stimulants. When the person stops drinking, the body tries to make up for lost time by producing more glutamine than it needs. The increase in glutamine levels stimulates the brain while the drinker is trying to sleep, keeping him/her from reaching the deepest levels of sleep.[318] Stopping chronic alcohol use can also lead to severe insomnia with vivid dreams. During withdrawal REM sleep is typically exaggerated as part of a rebound effect.[186]
Health effects of moderate drinking
Longevity
A meta-analysis found with data from 477,200 individuals determined the dose-response relationships by sex and end point using lifetime abstainers as the reference group. The search revealed 20 cohort studies that met our inclusion criteria. A U-shaped relationship was found for both sexes. Compared with lifetime abstainers, the relative risk (RR) for type 2 diabetes among men was most protective when consuming 22 g/day alcohol (RR 0.87 [95% CI 0.76–1.00]) and became deleterious at just over 60 g/day alcohol (1.01 [0.71–1.44]). Among women, consumption of 24 g/day alcohol was most protective (0.60 [0.52–0.69]) and became deleterious at about 50 g/day alcohol (1.02 [0.83–1.26]).[319]
Interestingly, ethanol has been found to double the lifespans of worms feed 0.005% ethanol but does not markedly increase at higher concentrations. Supplementing starved cultures with n-propanol and n-butanol also extended lifespan.; 1-Propanol (n-propanol) is thought to be similar to ethanol in its effects on human body, but 2-4 times more potent. However, this seems to be statistically significant for humans when compared to the previous study discusses; Human macronutrients in food consist mainly of water and the Dietary Reference Intake (DRI) for water is 3.7 litres (3700 mL x 0.005% EtOH = 18.5 mL EtOH) for 19-70 year old males, and 2.7 litres (2700 mL x 0.005% EtOH = 13.5 mL) for 19-70 year old women.
Because former drinkers may be inspired to abstain due to health concerns, they may actually be at increased risk of developing diabetes, known as the sick-quitter effect. Moreover, the balance of risk of alcohol consumption on other diseases and health outcomes, even at moderate levels of consumption, may outweigh the positive benefits with regard to diabetes.
Additionally, the way in which alcohol is consumed (i.e., with meals or bingeing on weekends) affects various health outcomes. Thus, it may be the case that the risk of diabetes associated with heavy alcohol consumption is due to consumption mainly on the weekend as opposed to the same amount spread over a week.[319] In the United Kingdom "advice on weekly consumption is avoided".
In a 2010 long-term study of an older population, the beneficial effects of moderate drinking were confirmed, but abstainers and heavy drinkers showed an increase of about 50% in mortality (even after controlling for confounding factors).[320]
Diabetes
Daily consumption of a small amount of pure alcohol by older women may slow or prevent the onset of diabetes by lowering the level of blood glucose.[321] However, the researchers caution that the study used pure alcohol and that alcoholic beverages contain additives, including sugar, which would negate this effect.[321]
People with diabetes should avoid sugary drinks such as dessert wines and liqueurs.[322]
Heart disease
Alcohol consumption by the elderly results in increased longevity, which is almost entirely a result of lowered coronary heart disease.[323] A British study found that consumption of two units of alcohol (one regular glass of wine) daily by doctors aged 48+ years increased longevity by reducing the risk of death by ischaemic heart disease and respiratory disease.[324] Deaths for which alcohol consumption is known to increase risk accounted for only 5% of the total deaths, but this figure increased among those who drank more than two units of alcohol per day.[324]
One study found that men who drank moderate amounts of alcohol three or more times a week were up to 35% less likely to have a heart attack than non-drinkers, and men who increased their daily alcohol consumption by one drink over the 12 years of the study had a 22% lower risk of heart attack.[325]
Daily intake of one or two units of alcohol (a half or full standard glass of wine) is associated with a lower risk of coronary heart disease in men over 40, and in women who have been through menopause.[326] However, getting drunk one or more times per month put women at a significantly increased risk of heart attack, negating alcohol's potential protective effect.[327]
Increased longevity due to alcohol consumption is almost entirely the result of a reduced rate of coronary heart disease.[323]
Stroke
A study found that lifelong abstainers were 2.36 times more likely to suffer a stroke than those who regularly drank a moderate amount of alcohol beverages. Heavy drinkers were 2.88 times more likely to suffer a stroke than moderate drinkers.[328]
References
- ^ Meyer, Jerold S. and Linda F. Quenzer. Psychopharmacology: Drugs, the Brain, and Behavior. Sinauer Associates, Inc: Sunderland, Massachusetts. 2005. Page 228.
- ^ helsinki.fi - Effect of alcohol on hormones in women, Helsinki 2001
- ^ helsinki.fi - Clinical studies on dependence and drug effects, ESBRA 2009
- ^ a b Grattan, Karen E.; Vogel-Sprott, M. (2001). "Maintaining Intentional Control of Behavior Under Alcohol". Alcoholism: Clinical and Experimental Research. 25 (2): 192–7. doi:10.1111/j.1530-0277.2001.tb02198.x. PMID 11236832.
- ^ a b MacAndrew, C. and Edgerton. Drunken Comportment: A Social Explanation. Chicago: Aldine, 1969.
- ^ Marlatt, G. A.; Rosenow (1981). "The think-drink effect". Psychology Today. 15: 60–93.
{{cite journal}}: Cite has empty unknown parameter:|author-name-separator=(help); Unknown parameter|author-separator=ignored (help) - ^ "Alcohol". New World Encyclopedia. Retrieved 2013-02-05.
- ^ "Online Etymology Dictionary". Etymonline.com. Retrieved 2013-02-05.
- ^ "Sensible Drinking". Aim-digest.com. Retrieved 2013-02-05.
- ^ "Alcohol misuse : Department of Health". Dh.gov.uk. Retrieved 2013-02-05.
- ^ "Alcohol and health: how alcohol can affect your long and short term health". Drinkaware.co.uk. Retrieved 2013-02-05.
- ^ Drink limits ‘useless’, The Times, 20 October 2007
- ^ "Lexicon and drug terms". Who.int. 2010-12-09. Retrieved 2013-02-05.
- ^ "Scientific grounding for sobriety: Western experience" (PDF). 2010. Retrieved 2013-02-05.
{{cite web}}: Cite uses deprecated parameter|authors=(help) - ^ "TWELVE STEPS and TWELVE TRADITIONS"[dead link]
- ^ "Alcohol-Attributable Deaths and Years of Potential Life Lost — United States, 2001". Centers for Disease Control and Prevention. 2004-09-24.
- ^ "Alcohol". BBC News. 2000-08-09.
- ^ "Alcohol linked to thousands of deaths". BBC News. 2000-07-14.
- ^ a b "Burden of alcohol-related cancer substantial". Abramson Cancer Center of the University of Pennsylvania. 2006-08-03.
- ^ a b c d e "Alcohol and cancer". Cancer Research UK.
- ^ Attention: This template ({{cite pmid}}) is deprecated. To cite the publication identified by PMID 17382831, please use {{cite journal}} with
|pmid=17382831instead. - ^ "Drugs that cause most harm: Scoring drugs". The Economist. 2010-11-02. Retrieved 2013-02-05.
- ^ "Rs671".
- ^ Hui Li; et al. (2009). "Refined Geographic Distribution of the Oriental ALDH2*504Lys (nee 487Lys) Variant". Ann Hum Genet. 73 (Pt 3): 335–45. doi:10.1111/j.1469-1809.2009.00517.x. PMC 2846302. PMID 19456322.
{{cite journal}}: Explicit use of et al. in:|author=(help) - ^ Yi Peng, Hong Shi, Xue-bin Qi, Chun-jie Xiao, Hua Zhong, Run-lin Z Ma, Bing Su (2010). "The ADH1B Arg47His polymorphism in East Asian populations and expansion of rice domestication in history". BMC Evolutionary Biology. 10: 15. doi:10.1186/1471-2148-10-15. PMC 2823730. PMID 20089146.
{{cite journal}}: CS1 maint: multiple names: authors list (link) CS1 maint: unflagged free DOI (link) - ^ Oota; et al. (2004). "The evolution and population genetics of the ALDH2 locus: random genetic drift, selection, and low levels of recombination". Annals of Human Genetics.
{{cite journal}}: Explicit use of et al. in:|author=(help) - ^ "Women & Alcohol: The Hidden Risks of Drinking". Helpguide.org. Retrieved 2013-02-05.
- ^ http://www.ncbi.nlm.nih.gov/pubmed/8872236
- ^ “Antidepressants Help Men, But Not Women, Decrease Alcohol Consumption.” Science Daily. Feb. 27, 2007.
- ^ Graham, Katherine and Massak, Agnes. “Alcohol consumption and the use of antidepressants.” UK Pubmed Central (2007). June 20, 2012.
- ^ Horowitz M, Maddox A, Bochner M; et al. (1989). "Relationships between gastric emptying of solid and caloric liquid meals and alcohol absorption". Am. J. Physiol. 257 (2 Pt 1): G291–8. PMID 2764113.
{{cite journal}}: Explicit use of et al. in:|author=(help); Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ http://ask.yahoo.com/20020805.html
- ^ Alcohol Awareness Page
- ^ Carleton College: Wellness Center: Blood Alcohol Concentration (BAC)
- ^ a b c Feige B, Scaal S, Hornyak M, Gann H, Riemann D (2007). "Sleep electroencephalographic spectral power after withdrawal from alcohol in alcohol-dependent patients". Alcohol. Clin. Exp. Res. 31 (1): 19–27. doi:10.1111/j.1530-0277.2006.00260.x. PMID 17207097.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) Cite error: The named reference "ReferenceA" was defined multiple times with different content (see the help page). - ^ a b c d e f Roehrs T, Roth T (2001). "Sleep, sleepiness, and alcohol use". Alcohol Res Health. 25 (2): 101–9. PMID 11584549.
- ^ Stone BM (1980). "Sleep and low doses of alcohol". Electroencephalogr Clin Neurophysiol. 48 (6): 706–9. doi:10.1016/0013-4694(80)90427-7. PMID 6155259.
{{cite journal}}: Unknown parameter|month=ignored (help) - ^ Schuckit MA (1994). "Low level of response to alcohol as a predictor of future alcoholism". Am J Psychiatry. 151 (2): 184–9. PMID 8296886.
{{cite journal}}: Unknown parameter|month=ignored (help) - ^ Roehrs T, Papineau K, Rosenthal L, Roth T (1999). "Ethanol as a hypnotic in insomniacs: self administration and effects on sleep and mood". Neuropsychopharmacology. 20 (3): 279–86. doi:10.1016/S0893-133X(98)00068-2. PMID 10063488.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ Levine, M. E. (1994). "Fatigue, Sleep, and Seasonal Hormone Levels: Implications for Drinking Behavior in Northern Climates". Drugs & Society. 8 (2): 61–70.
{{cite journal}}: Unknown parameter|coauthors=ignored (|author=suggested) (help) - ^ a b Kühlwein E, Hauger RL, Irwin MR (2003). "Abnormal nocturnal melatonin secretion and disordered sleep in abstinent alcoholics". Biol. Psychiatry. 54 (12): 1437–43. doi:10.1016/S0006-3223(03)00005-2. PMID 14675809.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ Danel T, Libersa C, Touitou Y (2001). "The effect of alcohol consumption on the circadian control of human core body temperature is time dependent". Am. J. Physiol. Regul. Integr. Comp. Physiol. 281 (1): R52–5. PMID 11404278.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ [1], Why does my head spin when I'm drunk? Rachel Nuwer, 8 Feb 2011, Scienceline.
- ^ [2], Short Term Effects of Alcohol, citizendia.org.
- ^ a b c d e f Andréasson, S.; Allebeck, P. (28 February–6 March 2005). "[Alcohol as medication is no good. More risks than benefits according to a survey of current knowledge]". Lakartidningen. 102 (9): 632–7. PMID 15804034.
{{cite journal}}: Check date values in:|date=(help) Cite error: The named reference "Andréasson-" was defined multiple times with different content (see the help page). - ^ Grattan KE, Vogel-Sprott M (2001). "Maintaining intentional control of behavior under alcohol". Alcohol. Clin. Exp. Res. 25 (2): 192–7. doi:10.1111/j.1530-0277.2001.tb02198.x. PMID 11236832.
{{cite journal}}: Unknown parameter|month=ignored (help) - ^ Grant NK, Macdonald TK (2005). "Can alcohol lead to inhibition or disinhibition? Applying alcohol myopia to animal experimentation". Alcohol Alcohol. 40 (5): 373–8. doi:10.1093/alcalc/agh177. PMID 15996970.
- ^ http://www.sirc.org/publik/drinking4.html
- ^ Huang Q, He X, Ma C; et al. (2000). "Pharmacophore/receptor models for GABAA/BzR subtypes (α1β3γ2, α5β3γ2, and α6β3γ2) via a comprehensive ligand-mapping approach". J. Med. Chem. 43 (1): 71–95. doi:10.1021/jm990341r. PMID 10633039.
{{cite journal}}: Explicit use of et al. in:|author=(help); Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ Platt DM, Duggan A, Spealman RD; et al. (2005). "Contribution of α1GABAA and α5GABAA receptor subtypes to the discriminative stimulus effects of ethanol in squirrel monkeys". J. Pharmacol. Exp. Ther. 313 (2): 658–67. doi:10.1124/jpet.104.080275. PMID 15650112.
{{cite journal}}: Explicit use of et al. in:|author=(help); Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ Duke AN, Platt DM, Cook JM; et al. (2006). "Enhanced sucrose pellet consumption induced by benzodiazepine-type drugs in squirrel monkeys: role of GABAA receptor subtypes". Psychopharmacology (Berl.). 187 (3): 321–30. doi:10.1007/s00213-006-0431-2. PMID 16783540.
{{cite journal}}: Explicit use of et al. in:|author=(help); Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ Wallner M, Hanchar HJ, Olsen RW (2006). "Low-dose alcohol actions on α4β3δ GABAA receptors are reversed by the behavioral alcohol antagonist Ro15-4513". Proc. Natl. Acad. Sci. U.S.A. 103 (22): 8540–5. doi:10.1073/pnas.0600194103. PMC 1482527. PMID 16698930.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ Mehta AK, Ticku MK (1988). "Ethanol potentiation of GABAergic transmission in cultured spinal cord neurons involves gamma-aminobutyric acidA-gated chloride channels". J. Pharmacol. Exp. Ther. 246 (2): 558–64. PMID 2457076.
{{cite journal}}: Unknown parameter|month=ignored (help) - ^ Becker HC, Anton RF (1989). "The benzodiazepine receptor inverse agonist RO15-4513 exacerbates, but does not precipitate, ethanol withdrawal in mice". Pharmacol. Biochem. Behav. 32 (1): 163–7. doi:10.1016/0091-3057(89)90227-X. PMID 2543989.
{{cite journal}}: Unknown parameter|month=ignored (help) - ^ Hanchar HJ, Chutsrinopkun P, Meera P; et al. (2006). "Ethanol potently and competitively inhibits binding of the alcohol antagonist Ro15-4513 to α4/6β3δ GABAA". Proc. Natl. Acad. Sci. U.S.A. 103 (22): 8546–51. doi:10.1073/pnas.0509903103. PMC 1482528. PMID 16581914.
{{cite journal}}: Explicit use of et al. in:|author=(help); Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ Shimizu, A. Matsubara, K. Uezono, T. Kimura, K. Shiono, H. "Reduced dorsal hippocampal glutamate release significantly correlates with the spatial memory deficits produced by benzodiazepines and ethanol". Neuroscience. P 701-706
- ^ Meyer, Jerrold. Quenzer, Linda. "Psychopharmacology: drugs brain and behavior"
- ^ Petrakis IL, Limoncelli D, Gueorguieva R; et al. (2004). "Altered NMDA glutamate receptor antagonist response in individuals with a family vulnerability to alcoholism". Am J Psychiatry. 161 (10): 1776–82. doi:10.1176/appi.ajp.161.10.1776. PMID 15465973.
{{cite journal}}: Explicit use of et al. in:|author=(help); Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ Nutt DJ (2006). "Alcohol alternatives—a goal for psychopharmacology?". J. Psychopharmacol. (Oxford). 20 (3): 318–20. doi:10.1177/0269881106063042. PMID 16574703.
{{cite journal}}: Unknown parameter|month=ignored (help) - ^ Qiang M, Denny AD, Ticku MK (2007). "Chronic intermittent ethanol treatment selectively alters N-methyl-D-aspartate receptor subunit surface expression in cultured cortical neurons". Mol. Pharmacol. 72 (1): 95–102. doi:10.1124/mol.106.033043. PMID 17440117.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ Hendricson AW, Maldve RE, Salinas AG; et al. (2007). "Aberrant synaptic activation of N-methyl-D-aspartate receptors underlies ethanol withdrawal hyperexcitability". J. Pharmacol. Exp. Ther. 321 (1): 60–72. doi:10.1124/jpet.106.111419. PMID 17229881.
{{cite journal}}: Explicit use of et al. in:|author=(help); Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ Dodd PR, Buckley ST, Eckert AL, Foley PF, Innes DJ (2006). "Genes and gene expression in the brains of human alcoholics". Ann. N. Y. Acad. Sci. 1074 (1): 104–15. doi:10.1196/annals.1369.010. PMID 17105908.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ Sircar R, Sircar D (2006). "Repeated ethanol treatment in adolescent rats alters cortical NMDA receptor". Alcohol. 39 (1): 51–8. doi:10.1016/j.alcohol.2006.07.002. PMID 16938629.
{{cite journal}}: Unknown parameter|month=ignored (help) - ^ Klein G, Gardiwal A, Schaefer A, Panning B, Breitmeier D (2007). "Effect of ethanol on cardiac single sodium channel gating". Forensic Sci. Int. 171 (2–3): 131–5. doi:10.1016/j.forsciint.2006.10.012. PMID 17129694.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ Shiraishi M, Harris RA (2004). "Effects of alcohols and anesthetics on recombinant voltage-gated Na+ channels". J. Pharmacol. Exp. Ther. 309 (3): 987–94. doi:10.1124/jpet.103.064063. PMID 14978193.
{{cite journal}}: Unknown parameter|month=ignored (help) - ^ DeGrandpre, Richard J.; Bickel, Warren K. (1996). Drug Policy and Human Nature: Psychological Perspectives on the Prevention, Management, and Treatment of Illicit Drug Abuse. New York: Plenum Press. ISBN 0-306-45241-3.
{{cite book}}: CS1 maint: multiple names: authors list (link) - ^ Latest Buzz in Research: Intoxicated Honey bees may clue Scientists into Drunken Human Behavior, The Ohio State Research News, Research Communications, Columbus OH, 23 October 2004.
- ^ Abramson CI, Stone SM, Ortez RA; et al. (2000). "The development of an ethanol model using social insects I: behavior studies of the honey bee (Apis mellifera L.)". Alcohol. Clin. Exp. Res. 24 (8): 1153–66. doi:10.1111/j.1530-0277.2000.tb02078.x. PMID 10968652.
{{cite journal}}: Explicit use of et al. in:|author=(help); Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ Intoxicated Honey Bees May Clue Scientists Into Drunken Human Behavior, Science Daily, 25 October 2004
- ^ Abramson CI, Fellows GW, Browne BL, Lawson A, Ortiz RA (2003). "Development of an ethanol model using social insects: II. Effect of Antabuse on consumatory responses and learned behavior of the honey bee (Apis mellifera L.)". Psychol Rep. 92 (2): 365–78. doi:10.2466/PR0.92.2.365-378. PMID 12785614.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ A hybridizing of effects as described at Alcohol's Effects from Virginia Tech and Federal Aviation Regulation (CFR) 91.17: Alcohol and Flying (hosted on FlightPhysical.com)
- ^ BAC Charts from Virginia Tech
- ^ a b "Quick Stats: Binge Drinking." The Centers for Disease Control and Prevention. April 2008.[3].
- ^ Based on the CDC standard of 0.6 fl oz alcohol per drink. CDC alcohol FAQ
- ^ <http://flightphysical.com/pilot/alcohol.htm/
- ^ http://info.insure.com/auto/baccalc.html
- ^ a b Andersson, Agneta; Wiréhn, Ann-Britt; Ölvander, Christina; Ekman, Diana; Bendtsen, Preben (2009). "Alcohol use among university students in Sweden measured by an electronic screening instrument". BMC Public Health. 9: 229. doi:10.1186/1471-2458-9-229. PMC 2724514. PMID 19594906.
{{cite journal}}: CS1 maint: unflagged free DOI (link) - ^ Cowan Jr, JM; Weathermon, A; McCutcheon, JR; Oliver, RD (1996). "Determination of volume of distribution for ethanol in male and female subjects". Journal of analytical toxicology. 20 (5): 287–90. doi:10.1093/jat/20.5.287. PMID 8872236.
{{cite journal}}: Unknown parameter|doi_brokendate=ignored (|doi-broken-date=suggested) (help) - ^ Biological Effects of Alcohol Use, Michaele Dunlap, Psy.D
- ^ G. Harding "A Wine Miscellany" pg 136–137, Clarkson Potter Publishing, New York 2005 ISBN 0-307-34635-8
- ^ Global Status Report on Alcohol 2004
- ^ Association of alcohol consumption with selected cardiovascular disease outcomes: a systematic review and meta-analysis. Paul E Ronksley, Susan E Brien, Barbara J Turner, Kenneth J Mukamal, William A Ghali BMJ 2011;342:d671
- ^ Prospective study of alcohol drinking patterns and coronary heart disease in women and men. Janne Tolstrup, Majken K Jensen, Tjønneland Anne, Kim Overvad, Kenneth J Mukamal, and Morten Grønbæk. BMJ 2006;332:1244.
- ^ No authors listed (2000). "Health Risks and Benefits of Alcohol Consumption Health Risks and Benefits of Alcohol Consumption". Alcohol Res Health 24 (1): 5–11.
- ^ Müller D, Koch RD, von Specht H, Völker W, Münch EM (1985). "[Neurophysiologic findings in chronic alcohol abuse]". Psychiatr Neurol Med Psychol (Leipz) (in German). 37 (3): 129–32. PMID 2988001.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ Testino G (2008). "Alcoholic diseases in hepato-gastroenterology: a point of view". Hepatogastroenterology. 55 (82–83): 371–7. PMID 18613369.
- ^ Caan, Woody; Belleroche, Jackie de, eds. (11 April 2002). Drink, Drugs and Dependence: From Science to Clinical Practice (1st ed.). Routledge. pp. 19–20. ISBN 978-0-415-27891-1.
- ^ Mellon, RD.; Simone, AF.; Rappaport, BA. (2007). "Use of anesthetic agents in neonates and young children". Anesth Analg. 104 (3): 509–20. doi:10.1213/01.ane.0000255729.96438.b0. PMID 17312200.
{{cite journal}}: Unknown parameter|month=ignored (help) - ^ Cabot, R.C. (1904). "The relation of alcohol to arterioscleroisis". Journal of the American Medical Association. 43: 774–775.
- ^ a b Sellman, D.; Connor, J.; Robinson, G.; Jackson, R. (2009). "Alcohol cardio-protection has been talked up". N Z Med J. 122 (1303): 97–101. PMID 19851424.
- ^ Sinkiewicz, W.; Weglarz, M. (2009). "[Alcohol and wine and cardiovascular diseases in epidemiologic studies]". Przegl Lek. 66 (5): 233–8. PMID 19739580.
- ^ Gitlow, Stuart (1 October 2006). Substance Use Disorders: A Practical Guide (2nd ed.). USA: Lippincott Williams and Wilkins. pp. 101–103. ISBN 978-0-7817-6998-3.
- ^ Taylor B, Rehm J, Gmel G (2005). "Moderate alcohol consumption and the gastrointestinal tract". Dig Dis. 23 (3–4): 170–6. doi:10.1159/000090163. PMID 16508280.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Cargiulo T (2007). "Understanding the health impact of alcohol dependence". Am J Health Syst Pharm. 64 (5 Suppl 3): S5–11. doi:10.2146/ajhp060647. PMID 17322182.
{{cite journal}}: Unknown parameter|month=ignored (help) - ^ Stevenson JS (2005). "Alcohol use, misuse, abuse, and dependence in later adulthood". Annu Rev Nurs Res. 23: 245–80. PMID 16350768.
- ^ Vliegenthart R, Oei HH, van den Elzen AP; et al. (2004). "Alcohol consumption and coronary calcification in a general population". Arch. Intern. Med. 164 (21): 2355–60. doi:10.1001/archinte.164.21.2355. PMID 15557415.
{{cite journal}}: Explicit use of et al. in:|author=(help); Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link)
Koppes LL, Twisk JW, Snel J, Van Mechelen W, Kemper HC (2000). "Blood cholesterol levels of 32-year-old alcohol consumers are better than of nonconsumers". Pharmacol Biochem Behav. 66 (1): 163–7. doi:10.1016/S0091-3057(00)00195-7. PMID 10837856.{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link)
Albert MA, Glynn RJ, Ridker PM (2003). "Alcohol consumption and plasma concentration of C-reactive protein". Circulation. 107 (3): 443–7. doi:10.1161/01.CIR.0000045669.16499.EC. PMID 12551869.{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link)
Baer DJ, Judd JT, Clevidence BA; et al. (1 March 2002). "Moderate alcohol consumption lowers risk factors for cardiovascular disease in postmenopausal women fed a controlled diet". Am J Clin Nutr. 75 (3): 593–9. PMID 11864868.{{cite journal}}: Explicit use of et al. in:|author=(help)CS1 maint: multiple names: authors list (link) - ^ Catena C, Novello M, Dotto L, De Marchi S, Sechi LA (2003). "Serum lipoprotein(a) concentrations and alcohol consumption in hypertension: possible relevance for cardiovascular damage". J. Hypertens. 21 (2): 281–8. doi:10.1097/01.hjh.0000052436.12292.26. PMID 12569257.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ Lopez AD, Mathers CD, Ezzati M, Jamison DT, Murray CJ (2006). "Global and regional burden of disease and risk factors, 2001: systematic analysis of population health data". Lancet. 367 (9524): 1747–57. doi:10.1016/S0140-6736(06)68770-9. PMID 16731270.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ BBC Alcohol link to one in 25 deaths
- ^ Jürgen Rehm, Colin Mathers, Svetlana Popova, Montarat Thavorncharoensap, Yot Teerawattananon, Jayadeep Patra Global burden of disease and injury and economic cost attributable to alcohol use and alcohol-use disorders The Lancet, Volume 373, Issue 9682, Pages 2223 - 2233, 27 June 2009 doi:10.1016/S0140-6736(09)60746-7
- ^ IARC Alcohol causes more than half of all the premature deaths in Russian adults
- ^ Tjønneland, A.; Christensen, J.; Olsen, A.; Stripp, C.; Thomsen, BL.; Overvad, K.; Peeters, PH.; van Gils, CH.; Bueno-de-Mesquita, HB. (2007). "Alcohol intake and breast cancer risk: the European Prospective Investigation into Cancer and Nutrition (EPIC)". Cancer Causes Control. 18 (4): 361–73. doi:10.1007/s10552-006-0112-9. PMID 17364225.
{{cite journal}}: Unknown parameter|month=ignored (help) - ^ Soerjomataram, I.; de Vries, E.; Coebergh, JW. (2009). "Did alcohol protect against death from breast cancer in Russia?". Lancet. 374 (9694): 975, author reply 975–6. doi:10.1016/S0140-6736(09)61657-3. PMID 19766875.
{{cite journal}}: Unknown parameter|month=ignored (help) - ^ Alcohol-related deaths in the United Kingdom and links therefrom
- ^ Alcohol Deaths: Rates stabilise in the UK
- ^ BBC Alcohol 'kills one in 20 Scots' 30 June 2009
- ^ Sam Lister The price of alcohol: an extra 6,000 early deaths a year The Times, 19 October 2009
- ^ Centers for Disease Control and Prevention Alcohol and Public Health
- ^ McGinnis, J. Michael; Foege, William H. (1993). "Actual Causes of Death in the United States". JAMA. 270 (18): 2207–2212. doi:10.1001/jama.270.18.2207. PMID 8411605.
{{cite journal}}: Unknown parameter|author-separator=ignored (help) - ^ Di Castelnuovo A, Costanzo S, Bagnardi V, Donati MB, Iacoviello L, de Gaetano G. Alcohol dosing and total mortality in men and women: an updated meta-analysis of 34 prospective studies. Arch Intern Med. 2006 Dec 11-25;166(22):2437-45.
- ^ http://www.drinkaware.co.uk/facts/frequently-asked-questions#what_is_unit
- ^ a b Doll R, Peto R, Boreham J, Sutherland I (2005). "Mortality in relation to alcohol consumption: a prospective study among male British doctors". Int J Epidemiol. 34 (1): 199–204. doi:10.1093/ije/dyh369. PMID 15647313.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ a b Di Castelnuovo, A.; Costanzo, S.; Bagnardi, V.; Donati, MB.; Iacoviello, L.; de Gaetano, G. "Alcohol dosing and total mortality in men and women: an updated meta-analysis of 34 prospective studies". Arch Intern Med. 166 (22): 2437–45. doi:10.1001/archinte.166.22.2437. PMID 17159008. Cite error: The named reference "Di Castelnuovo-" was defined multiple times with different content (see the help page).
- ^ Fillmore, KM.; Stockwell, T.; Chikritzhs, T.; Bostrom, A.; Kerr, W. (2007). "Moderate alcohol use and reduced mortality risk: systematic error in prospective studies and new hypotheses". Ann Epidemiol. 17 (5 Suppl): S16-23. doi:10.1016/j.annepidem.2007.01.005. PMID 17478320.
{{cite journal}}: Unknown parameter|month=ignored (help) - ^ Chikritzhs, T.; Fillmore, K.; Stockwell, T. (2009). "A healthy dose of scepticism: four good reasons to think again about protective effects of alcohol on coronary heart disease". Drug Alcohol Rev. 28 (4): 441–4. doi:10.1111/j.1465-3362.2009.00052.x. PMID 19594799.
{{cite journal}}: Unknown parameter|month=ignored (help) - ^ a b Ann Epidemiol. 2007. Volume 17, Issue 5. Alcohol Drinking and Total Mortality Risk Arthur L. Klatsky, MD, Natalia Udaltsova, PhD
- ^ a b Lee, SJ.; Sudore, RL.; Williams, BA.; Lindquist, K.; Chen, HL.; Covinsky, KE. (2009). "Functional limitations, socioeconomic status, and all-cause mortality in moderate alcohol drinkers". J Am Geriatr Soc. 57 (6): 955–62. doi:10.1111/j.1532-5415.2009.02184.x. PMID 19473456.
{{cite journal}}: Unknown parameter|month=ignored (help) - ^ Arriola, L.; Martinez-Camblor, P.; Larrañaga, N.; Basterretxea, M.; Amiano, P.; Moreno-Iribas, C.; Carracedo, R.; Agudo, A.; Ardanaz, E. (2010). "Alcohol intake and the risk of coronary heart disease in the Spanish EPIC cohort study". Heart. 96 (2): 124–30. doi:10.1136/hrt.2009.173419. PMID 19933099.
{{cite journal}}: Unknown parameter|month=ignored (help) - ^ a b c d Holahan, CJ.; Schutte, KK.; Brennan, PL.; Holahan, CK.; Moos, BS.; Moos, RH. (2010). "Late-life alcohol consumption and 20-year mortality". Alcohol Clin Exp Res. 34 (11): 1961–71. doi:10.1111/j.1530-0277.2010.01286.x. PMID 20735372.
{{cite journal}}: Unknown parameter|month=ignored (help) - ^ Hansel, B.; Thomas, F.; Pannier, B.; Bean, K.; Kontush, A.; Chapman, MJ.; Guize, L.; Bruckert, E. (2010). "Relationship between alcohol intake, health and social status and cardiovascular risk factors in the urban Paris-Ile-De-France Cohort: is the cardioprotective action of alcohol a myth?". Eur J Clin Nutr. 64 (6): 561–8. doi:10.1038/ejcn.2010.61. PMID 20485310.
{{cite journal}}: Unknown parameter|month=ignored (help) - ^ Klatsky, AL. (2008). "Invited commentary: never, or hardly ever? It could make a difference". Am J Epidemiol. 168 (8): 872–5, discussion 876–7. doi:10.1093/aje/kwn192. PMID 18701441.
{{cite journal}}: Unknown parameter|month=ignored (help) - ^ Laatikainen, T.; Manninen, L.; Poikolainen, K.; Vartiainen, E. (2003). "Increased mortality related to heavy alcohol intake pattern". J Epidemiol Community Health. 57 (5): 379–84. PMC 1732462. PMID 12700224.
{{cite journal}}: Unknown parameter|month=ignored (help) - ^ "Risk Factors for Early Myocardial Infarction in South Asians Compared With Individuals in Other Countries" (PDF). JAMA. 297 (3). American Medical Association: 286–294. 17. Retrieved 20 March 2012.
{{cite journal}}: Check date values in:|date=and|year=/|date=mismatch (help); Unknown parameter|coauthors=ignored (|author=suggested) (help); Unknown parameter|month=ignored (help) - ^ a b c "Impact of alcohol on coronary heart disease in Indian men". Atherosclerosis. 210 (2): 531–535. 26. doi:10.1016/j.atherosclerosis.2010.02.033. PMID 20226461.
{{cite journal}}:|access-date=requires|url=(help); Check date values in:|date=and|year=/|date=mismatch (help); Unknown parameter|coauthors=ignored (|author=suggested) (help); Unknown parameter|month=ignored (help)CS1 maint: extra punctuation (link) - ^ Mennen LI, Balkau B, Vol S, Cacès E, Eschwège E (1 April 1999). "Fibrinogen: a possible link between alcohol consumption and cardiovascular disease? DESIR Study Group". Arterioscler Thromb Vasc Biol. 19 (4): 887–92. PMID 10195914.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Paassilta M, Kervinen K, Rantala AO; et al. (14 February 1998). "Social alcohol consumption and low Lp(a) lipoprotein concentrations in middle aged Finnish men: population based study". BMJ. 316 (7131): 594–5. PMC 28464. PMID 9518912.
{{cite journal}}: Explicit use of et al. in:|author=(help)CS1 maint: multiple names: authors list (link) - ^ Lacoste L, Hung J, Lam JY (2001). "Acute and delayed antithrombotic effects of alcohol in humans". Am J Cardiol. 87 (1): 82–5. doi:10.1016/S0002-9149(00)01277-7. PMID 11137839.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link)
Pahor M, Guralnik JM, Havlik RJ; et al. (1996). "Alcohol consumption and risk of deep venous thrombosis and pulmonary embolism in older persons". J Am Geriatr Soc. 44 (9): 1030–7. PMID 8790226.{{cite journal}}: Explicit use of et al. in:|author=(help); Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link)
Ridker, P., et al. Moderate alcohol intake may reduce risk of thrombosis. American Medical Association press release, September 22, 1994
Ridker, P. (1996). "The Pathogenesis of Atherosclerosis and Acute Thrombosis". In Manson, JoAnn E. (ed.). Prevention of myocardial infarction. Oxford [Oxfordshire]: Oxford University Press. ISBN 0-19-508582-5. - ^ Rimm, EB.; Williams, P.; Fosher, K.; Criqui, M.; Stampfer, MJ. (1999). "Moderate alcohol intake and lower risk of coronary heart disease: meta-analysis of effects on lipids and haemostatic factors". BMJ. 319 (7224): 1523–8. PMC 28294. PMID 10591709.
{{cite journal}}: Unknown parameter|month=ignored (help) - ^ Albert, MA.; Glynn, RJ.; Ridker, PM. (2003). "Alcohol consumption and plasma concentration of C-reactive protein". Circulation. 107 (3): 443–7. doi:10.1161/01.CIR.0000045669.16499.EC. PMID 12551869.
{{cite journal}}: Unknown parameter|month=ignored (help) - ^ Stewart, SH.; Mainous, AG.; Gilbert, G. (2002). "Relation between alcohol consumption and C-reactive protein levels in the adult US population" (PDF). J Am Board Fam Pract. 15 (6): 437–42. PMID 12463288.
- ^ Imhof, A.; Froehlich, M.; Brenner, H.; Boeing, H.; Pepys, MB.; Koenig, W. (2001). "Effect of alcohol consumption on systemic markers of inflammation". Lancet. 357 (9258): 763–7. doi:10.1016/S0140-6736(00)04170-2. PMID 11253971.
{{cite journal}}: Unknown parameter|month=ignored (help) - ^ Abdulla S (1997). "Is alcohol really good for you?". J R Soc Med. 90 (12): 651. PMC 1296731. PMID 9496287.
{{cite journal}}: Unknown parameter|month=ignored (help) - ^ Naimi TS, Brown DW, Brewer RD; et al. (2005). "Cardiovascular risk factors and confounders among nondrinking and moderate-drinking U.S. adults". Am J Prev Med. 28 (4): 369–73. doi:10.1016/j.amepre.2005.01.011. PMID 15831343.
{{cite journal}}: Explicit use of et al. in:|author=(help); Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ Vogel, RA. (2002). "Alcohol, heart disease, and mortality: a review". Rev Cardiovasc Med. 3 (1): 7–13. PMID 12439349.
- ^ Sesso HD, Stampfer MJ, Rosner B, Hennekens CH, Manson JE, Gaziano JM (2000). "Seven-Year Changes in Alcohol Consumption and Subsequent Risk of Cardiovascular Disease in Men". Arch Intern Med. 160 (17): 2605–12. doi:10.1001/archinte.160.17.2605. PMID 10999974.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Camargo CA, Stampfer MJ, Glynn RJ; et al. (4 February 1997). "Prospective study of moderate alcohol consumption and risk of peripheral arterial disease in US male physicians". Circulation. 95 (3): 577–80. PMID 9024142.
{{cite journal}}: Explicit use of et al. in:|author=(help)CS1 maint: multiple names: authors list (link) - ^ Vliegenthart R, Geleijnse JM, Hofman A; et al. (2002). "Alcohol consumption and risk of peripheral arterial disease: the Rotterdam study". Am J Epidemiol. 155 (4): 332–8. doi:10.1093/aje/155.4.332. PMID 11836197.
{{cite journal}}: Explicit use of et al. in:|author=(help); Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ Mingardi R, Avogaro A, Noventa F; et al. (1997). "Alcohol intake is associated with a lower prevalence of peripheral vascular disease in non-insulin dependent diabetic women". Nutrition Metabolism and Cardiovascular Disease. 7 (4): 301–8.
{{cite journal}}: Explicit use of et al. in:|author=(help)CS1 maint: multiple names: authors list (link) - ^ Djoussé L, Levy D, Murabito JM, Cupples LA, Ellison RC (19 December 2000). "Alcohol consumption and risk of intermittent claudication in the Framingham Heart Study". Circulation. 102 (25): 3092–7. PMID 11120700.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Muntwyler J, Hennekens CH, Buring JE, Gaziano JM (1998). "Mortality and light to moderate alcohol consumption after myocardial infarction". Lancet. 352 (9144): 1882–5. doi:10.1016/S0140-6736(98)06351-X. PMID 9863785.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ Mukamal KJ, Maclure M, Muller JE, Sherwood JB, Mittleman MA (2001). "Prior alcohol consumption and mortality following acute myocardial infarction". JAMA. 285 (15): 1965–70. doi:10.1001/jama.285.15.1965. PMID 11308432.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ Alcohol helps reduce damage after heart attacks
- ^ Djoussé L, Gaziano JM (2008). "Alcohol consumption and heart failure: a systematic review". Curr Atheroscler Rep. 10 (2): 117–20. doi:10.1007/s11883-008-0017-z. PMC 2365733. PMID 18417065.
{{cite journal}}: Unknown parameter|month=ignored (help) - ^ Kloner RA, Rezkalla SH (2007). "To drink or not to drink? That is the question". Circulation. 116 (11): 1306–17. doi:10.1161/CIRCULATIONAHA.106.678375. PMID 17846344.
{{cite journal}}: Unknown parameter|month=ignored (help) - ^ Saremi A, Arora R (2008). "The cardiovascular implications of alcohol and red wine". Am J Ther. 15 (3): 265–77. doi:10.1097/MJT.0b013e3180a5e61a. PMID 18496264.
- ^ Awtry, EH.; Philippides, GJ. (2010). "Alcoholic and cocaine-associated cardiomyopathies". Prog Cardiovasc Dis. 52 (4): 289–99. doi:10.1016/j.pcad.2009.11.004. PMID 20109599.
- ^ Savage D, Lindenbaum J (1986). "Anemia in alcoholics". Medicine (Baltimore). 65 (5): 322–38. PMID 3747828.
- ^ Panza F, Capurso C, D'Introno A; et al. (2008). "Vascular risk factors, alcohol intake, and cognitive decline". J Nutr Health Aging. 12 (6): 376–81. doi:10.1007/BF02982669. PMID 18548174.
{{cite journal}}: Explicit use of et al. in:|author=(help)CS1 maint: multiple names: authors list (link) - ^ Panza, F.; Capurso, C.; D'Introno, A.; Colacicco, AM.; Frisardi, V.; Lorusso, M.; Santamato, A.; Seripa, D.; Pilotto, A. (2009). "Alcohol drinking, cognitive functions in older age, predementia, and dementia syndromes". J Alzheimers Dis. 17 (1): 7–31. doi:10.3233/JAD-2009-1009. PMID 19494429.
{{cite journal}}: Unknown parameter|month=ignored (help) - ^ Verbaten, MN. (2009). "Chronic effects of low to moderate alcohol consumption on structural and functional properties of the brain: beneficial or not?". Hum Psychopharmacol. 24 (3): 199–205. doi:10.1002/hup.1022. PMID 19330800.
{{cite journal}}: Unknown parameter|month=ignored (help) - ^ Bleich S, Bleich K, Kropp S; et al. (2001). "Moderate alcohol consumption in social drinkers raises plasma homocysteine levels: a contradiction to the 'French Paradox'?". Alcohol Alcohol. 36 (3): 189–92. PMID 11373253.
{{cite journal}}: Explicit use of et al. in:|author=(help)CS1 maint: multiple names: authors list (link) - ^ Bleich S, Carl M, Bayerlein K; et al. (2005). "Evidence of increased homocysteine levels in alcoholism: the Franconian alcoholism research studies (FARS)". Alcohol. Clin. Exp. Res. 29 (3): 334–6. PMID 15770107.
{{cite journal}}: Explicit use of et al. in:|author=(help); Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ Bleich S, Degner D, Bandelow B, von Ahsen N, Rüther E, Kornhuber J (2000). "Plasma homocysteine is a predictor of alcohol withdrawal seizures". NeuroReport. 11 (12): 2749–52. PMID 10976956.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ Bleich S, Bandelow B, Javaheripour K; et al. (2003). "Hyperhomocysteinemia as a new risk factor for brain shrinkage in patients with alcoholism". Neurosci. Lett. 335 (3): 179–82. doi:10.1016/S0304-3940(02)01194-1. PMID 12531462.
{{cite journal}}: Explicit use of et al. in:|author=(help); Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ Wilhelm J, Bayerlein K, Hillemacher T; et al. (2006). "Short-term cognition deficits during early alcohol withdrawal are associated with elevated plasma homocysteine levels in patients with alcoholism". J Neural Transm. 113 (3): 357–63. doi:10.1007/s00702-005-0333-1. PMID 15997414.
{{cite journal}}: Explicit use of et al. in:|author=(help); Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ Di Castelnuovo, A.; Costanzo, S.; di Giuseppe, R.; de Gaetano, G.; Iacoviello, L. (2009). "Alcohol consumption and cardiovascular risk: mechanisms of action and epidemiologic perspectives". Future Cardiol. 5 (5): 467–77. doi:10.2217/fca.09.36. PMID 19715411.
{{cite journal}}: Unknown parameter|month=ignored (help) - ^ Klatsky, AL. (2009). "Alcohol and cardiovascular diseases". Expert Rev Cardiovasc Ther. 7 (5): 499–506. doi:10.1586/erc.09.22. PMID 19419257.
{{cite journal}}: Unknown parameter|month=ignored (help) - ^ Galimanis, A.; Mono, ML.; Arnold, M.; Nedeltchev, K.; Mattle, HP. (2009). "Lifestyle and stroke risk: a review". Curr Opin Neurol. 22 (1): 60–8. doi:10.1097/WCO.0b013e32831fda0e. PMID 19155763.
{{cite journal}}: Unknown parameter|month=ignored (help) - ^ O'Keefe, JH.; Bybee, KA.; Lavie, CJ. (2007). "Alcohol and cardiovascular health: the razor-sharp double-edged sword". J Am Coll Cardiol. 50 (11): 1009–14. doi:10.1016/j.jacc.2007.04.089. PMID 17825708.
{{cite journal}}: Unknown parameter|month=ignored (help) - ^ http://www.stroke.org/site/PageServer?pagename=Alcohol
- ^ Emberson, JR.; Bennett, DA. (2006). "Effect of alcohol on risk of coronary heart disease and stroke: causality, bias, or a bit of both?". Vasc Health Risk Manag. 2 (3): 239–49. PMC 1993990. PMID 17326330.
- ^ Neiman, J. (1998). "Alcohol as a risk factor for brain damage: neurologic aspects". Alcohol Clin Exp Res. 22 (7 Suppl): 346S–351S. doi:10.1111/j.1530-0277.1998.tb04389.x. PMID 9799959.
{{cite journal}}: Unknown parameter|month=ignored (help) - ^ Avellaneda Fernández, A.; Pérez Martín, A.; Izquierdo Martínez, M.; Arruti Bustillo, M.; Barbado Hernández, FJ.; de la Cruz Labrado, J.; Díaz-Delgado Peñas, R.; Gutiérrez Rivas, E.; Palacín Delgado, C. (2009). "Chronic fatigue syndrome: aetiology, diagnosis and treatment". BMC Psychiatry. 9 Suppl 1: S1. doi:10.1186/1471-244X-9-S1-S1. PMID 19857242.
{{cite journal}}: CS1 maint: unflagged free DOI (link) - ^ Tapert SF, Brown GG, Kindermann SS, Cheung EH, Frank LR, Brown SA (2001). "fMRI measurement of brain dysfunction in alcohol-dependent young women". Alcohol. Clin. Exp. Res. 25 (2): 236–45. doi:10.1111/j.1530-0277.2001.tb02204.x. PMID 11236838.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ Squeglia LM, Jacobus J, Tapert SF (2009). "The influence of substance use on adolescent brain development". Clin EEG Neurosci. 40 (1): 31–8. PMC 2827693. PMID 19278130.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ Brown SA, Tapert SF, Granholm E, Delis DC (2000). "Neurocognitive functioning of adolescents: effects of protracted alcohol use". Alcohol Clin Exp Res. 24 (2): 164–71. doi:10.1111/j.1530-0277.2000.tb04586.x. PMID 10698367.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ Attention: This template ({{cite pmid}}) is deprecated. To cite the publication identified by PMID 20113871, please use {{cite journal}} with
|pmid=20113871instead. - ^ a b Attention: This template ({{cite pmid}}) is deprecated. To cite the publication identified by PMID 16272348, please use {{cite journal}} with
|pmid=16272348instead. - ^ Attention: This template ({{cite pmid}}) is deprecated. To cite the publication identified by PMID 17284196, please use {{cite journal}} with
|pmid=17284196instead. - ^ Attention: This template ({{cite pmid}}) is deprecated. To cite the publication identified by PMID 18061674, please use {{cite journal}} with
|pmid=18061674instead. - ^ Attention: This template ({{cite pmid}}) is deprecated. To cite the publication identified by PMID 12704810, please use {{cite journal}} with
|pmid=12704810instead. - ^ Attention: This template ({{cite pmid}}) is deprecated. To cite the publication identified by PMID 19077056, please use {{cite journal}} with
|pmid=19077056instead. - ^ a b c Attention: This template ({{cite pmid}}) is deprecated. To cite the publication identified by PMID 19554644, please use {{cite journal}} with
|pmid=19554644instead. - ^ a b c Attention: This template ({{cite pmid}}) is deprecated. To cite the publication identified by PMID 20534463, please use {{cite journal}} with
|pmid=20534463instead. - ^ Heffernan, TM. (2008). "The impact of excessive alcohol use on prospective memory: a brief review". Curr Drug Abuse Rev. 1 (1): 36–41. doi:10.2174/1874473710801010036. PMID 19630703.
{{cite journal}}: Unknown parameter|month=ignored (help) - ^ Pierucci-Lagha A, Derouesné C (2003). "[Alcoholism and aging. 2. Alcoholic dementia or alcoholic cognitive impairment?]". Psychol Neuropsychiatr Vieil (in French). 1 (4): 237–49. PMID 15683959.
{{cite journal}}: Unknown parameter|month=ignored (help) - ^ Peters R, Peters J, Warner J, Beckett N, Bulpitt C (2008). "Alcohol, dementia and cognitive decline in the elderly: a systematic review". Age Ageing. 37 (5): 505–12. doi:10.1093/ageing/afn095. PMID 18487267.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ Claudia Cooper, Paul Bebbington, Howard Meltzer, Rachel Jenkins, Traolach Brugha, James Lindesay and Gill Livingston Alcohol in moderation, premorbid intelligence and cognition In Older Adults: results from the Psychiatric Morbidity Survey J Neurol Neurosurg Psychiatry doi:10.1136/jnnp.2008.163964
- ^ Ohta, S (2004). "Mitochondrial ALDH2 Deficiency as an Oxidative Stress". Annals of the New York Academy of Sciences. 1011: 36–44. doi:10.1196/annals.1293.004. PMID 15126281. Retrieved 2009-08-13.
{{cite journal}}: Unknown parameter|coauthors=ignored (|author=suggested) (help); Unknown parameter|month=ignored (help) - ^ Martin PR, Singleton CK, Hiller-Sturmhöfel S (2003). "The role of thiamine deficiency in alcoholic brain disease". Alcohol Res Health. 27 (2): 134–42. PMID 15303623.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Butters N (1981). "The Wernicke-Korsakoff syndrome: a review of psychological, neuropathological and etiological factors". Curr Alcohol. 8: 205–32. PMID 6806017.
- ^
Bain PG, Findley LJ, Thompson PD; et al. (1994). "A study of hereditary essential tremor". Brain. 117 ((Pt 4)): 805–24. doi:10.1093/brain/117.4.805. PMID 7922467.
{{cite journal}}: Explicit use of et al. in:|author=(help); Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link)
Lou JS, Jankovic J (1991). "Essential tremor: clinical correlates in 350 patients". Neurology. 41 (2 (Pt 1)): 234–8. PMID 1992367.{{cite journal}}: Unknown parameter|month=ignored (help)
Wasielewski PG, Burns JM, Koller WC (1998). "Pharmacologic treatment of tremor". Mov Disord. 13 (Suppl 3): 90–100. doi:10.1002/mds.870131316. PMID 9827602.{{cite journal}}: CS1 maint: multiple names: authors list (link)
Boecker H, Wills AJ, Ceballos-Baumann A; et al. (1996). "The effect of ethanol on alcohol-responsive essential tremor: a positron emission tomography study". Ann. Neurol. 39 (5): 650–8. doi:10.1002/ana.410390515. PMID 8619551.{{cite journal}}: Explicit use of et al. in:|author=(help); Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link)
"Setting a steady course for benign essential tremor". Johns Hopkins Med Lett Health After 50. 11 (10): 3. 1999. PMID 10586714.{{cite journal}}: Unknown parameter|month=ignored (help) - ^ Attention: This template ({{cite pmid}}) is deprecated. To cite the publication identified by PMID 20721919, please use {{cite journal}} with
|pmid=20721919instead. - ^ Attention: This template ({{cite pmid}}) is deprecated. To cite the publication identified by PMID 21640732, please use {{cite journal}} with
|pmid=21640732instead. - ^ Attention: This template ({{cite pmid}}) is deprecated. To cite the publication identified by PMID 17366267, please use {{cite journal}} with
|pmid=17366267instead. - ^ a b Lee-chiong, Teofilo (24 April 2008). Sleep Medicine: Essentials and Review. Oxford University Press, USA. p. 105. ISBN 0-19-530659-7. Cite error: The named reference "sleep_medicine_a04" was defined multiple times with different content (see the help page).
- ^ Fergusson DM, Boden JM, Horwood LJ (2009). "Tests of causal links between alcohol abuse or dependence and major depression". Arch. Gen. Psychiatry. 66 (3): 260–6. doi:10.1001/archgenpsychiatry.2008.543. PMID 19255375.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ Chignon JM, Cortes MJ, Martin P, Chabannes JP (1998). "[Attempted suicide and alcohol dependence: results of an epidemiologic survey]". Encephale (in French). 24 (4): 347–54. PMID 9809240.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Ayd, Frank J. (31 May 2000). Lexicon of psychiatry, neurology, and the neurosciences. Philadelphia: Lippincott-Williams Wilkins. p. 349. ISBN 978-0-7817-2468-5.
- ^ Appleby, Louis; Duffy, David; Ryan, Tony (25 Aug 2004). New Approaches to Preventing Suicide: A Manual For Practitioners. Jessica Kingsley Publishers. pp. 31–32. ISBN 978-1-84310-221-2.
- ^ Uekermann J, Daum I (2008). "Social cognition in alcoholism: a link to prefrontal cortex dysfunction?". Addiction. 103 (5): 726–35. doi:10.1111/j.1360-0443.2008.02157.x. PMID 18412750.
{{cite journal}}: Unknown parameter|month=ignored (help) - ^ Jasova D, Bob P, Fedor-Freybergh P (2007). "Alcohol craving, limbic irritability, and stress". Med Sci Monit. 13 (12): CR543–7. PMID 18049433. Retrieved 2008-05-13.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ Marinkovic K (2009). "Alcoholism and dampened temporal limbic activation to emotional faces". Alcohol Clin Exp Res. 33 (11): 1880–92. doi:10.1111/j.1530-0277.2009.01026.x. PMID 19673745.
{{cite journal}}: Unknown parameter|coauthors=ignored (|author=suggested) (help); Unknown parameter|month=ignored (help) - ^ Wetterling T (2000). "Psychopathology of alcoholics during withdrawal and early abstinence". Eur Psychiatry. 15 (8): 483–8. doi:10.1016/S0924-9338(00)00519-8. PMID 11175926.
{{cite journal}}: Unknown parameter|coauthors=ignored (|author=suggested) (help); Unknown parameter|month=ignored (help) - ^ Cowley DS (24). "Alcohol abuse, substance abuse, and panic disorder". Am J Med. 92 (1A): 41S–8S. doi:10.1016/0002-9343(92)90136-Y. PMID 1346485.
{{cite journal}}: Check date values in:|date=and|year=/|date=mismatch (help); Unknown parameter|month=ignored (help) - ^ Cosci F (2007). "Alcohol use disorders and panic disorder: a review of the evidence of a direct relationship". J Clin Psychiatry. 68 (6): 874–80. doi:10.4088/JCP.v68n0608. PMID 17592911.
{{cite journal}}: Unknown parameter|coauthors=ignored (|author=suggested) (help); Unknown parameter|month=ignored (help) - ^ a b Alcohol-Related Psychosis at eMedicine
- ^ Tien AY, Anthony JC (1990). "Epidemiological analysis of alcohol and drug use as risk factors for psychotic experiences". J. Nerv. Ment. Dis. 178 (8): 473–80. doi:10.1097/00005053-199017880-00001. PMID 2380692.
{{cite journal}}: Unknown parameter|month=ignored (help) - ^ Terra MB, Figueira I, Barros HM (2004). "Impact of alcohol intoxication and withdrawal syndrome on social phobia and panic disorder in alcoholic inpatients". Rev Hosp Clin Fac Med Sao Paulo. 59 (4): 187–92. doi:10.1590/S0041-87812004000400006. PMID 15361983.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ Cohen SI (1995). "Alcohol and benzodiazepines generate anxiety, panic and phobias". J R Soc Med. 88 (2): 73–7. PMC 1295099. PMID 7769598.
{{cite journal}}: Unknown parameter|month=ignored (help) - ^ Cordain L, Bryan ED, Melby CL, Smith MJ (1 April 1997). "Influence of moderate daily wine consumption on body weight regulation and metabolism in healthy free-living males". J Am Coll Nutr. 16 (2): 134–9. PMID 9100213.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Arif AA, Rohrer JE (2005). "Patterns of alcohol drinking and its association with obesity: data from the Third National Health and Nutrition Examination Survey, 1988-1994". BMC Public Health. 5: 126. doi:10.1186/1471-2458-5-126. PMC 1318457. PMID 16329757.
{{cite journal}}: CS1 maint: unflagged free DOI (link) - ^ National Institute on Alcohol Abuse and Alcoholism (NIAAA) (2000). "Health risks and benefits of alcohol consumption" (PDF). Alcohol Res Health. 24 (1): 5–11. PMID 11199274.
- ^ Bode C, Bode JC (1997). "Alcohol's role in gastrointestinal tract disorders" (PDF). Alcohol Health Res World. 21 (1): 76–83. PMID 15706765.
- ^ Freiberg MS, Cabral HJ, Heeren TC, Vasan RS, Curtis Ellison R (2004). "Alcohol consumption and the prevalence of the Metabolic Syndrome in the US.: a cross-sectional analysis of data from the Third National Health and Nutrition Examination Survey". Diabetes Care. 27 (12): 2954–9. doi:10.2337/diacare.27.12.2954. PMID 15562213.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ Yoon YS, Oh SW, Baik HW, Park HS, Kim WY (1 July 2004). "Alcohol consumption and the metabolic syndrome in Korean adults: the 1998 Korean National Health and Nutrition Examination Survey". Am. J. Clin. Nutr. 80 (1): 217–24. PMID 15213051.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ La Vecchia C, Decarli A, Ferraroni M, Negri E (1994). "Alcohol drinking and prevalence of self-reported gallstone disease in the 1983 Italian National Health Survey". Epidemiology. 5 (5): 533–6. PMID 7986868.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ Leitzmann MF, Giovannucci EL, Stampfer MJ; et al. (1999). "Prospective study of alcohol consumption patterns in relation to symptomatic gallstone disease in men". Alcohol Clin Exp Res. 23 (5): 835–41. doi:10.1111/j.1530-0277.1999.tb04191.x. PMID 10371403.
{{cite journal}}: Explicit use of et al. in:|author=(help); Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ Sahi T, Paffenbarger RS, Hsieh CC, Lee IM (1 April 1998). "Body mass index, cigarette smoking, and other characteristics as predictors of self-reported, physician-diagnosed gallbladder disease in male college alumni". Am J Epidemiol. 147 (7): 644–51. PMID 9554603.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Simon JA, Grady D, Snabes MC, Fong J, Hunninghake DB (1998). "Ascorbic acid supplement use and the prevalence of gallbladder disease. Heart & Estrogen-Progestin Replacement Study (HERS) Research Group". J Clin Epidemiol. 51 (3): 257–65. doi:10.1016/S0895-4356(97)80280-6. PMID 9495691.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ a b Barve A, Khan R, Marsano L, Ravindra KV, McClain C (2008). "Treatment of alcoholic liver disease" (PDF). Ann Hepatol. 7 (1): 5–15. PMID 18376362.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Fehér J, Lengyel G (2008). "Silymarin in the treatment of chronic liver diseases: past and future". Orv Hetil (in Hungarian). 149 (51): 2413–8. doi:10.1556/OH.2008.28519. PMID 19073452.
{{cite journal}}: Unknown parameter|month=ignored (help) - ^ Voigt MD (2005). "Alcohol in hepatocellular cancer". Clin Liver Dis. 9 (1): 151–69. doi:10.1016/j.cld.2004.10.003. PMID 15763234.
{{cite journal}}: Unknown parameter|month=ignored (help) - ^ Morgan TR, Mandayam S, Jamal MM (2004). "Alcohol and hepatocellular carcinoma". Gastroenterology. 127 (5 Suppl 1): S87–96. doi:10.1053/j.gastro.2004.09.020. PMID 15508108.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ Frossard JL, Steer ML, Pastor CM (2008). "Acute pancreatitis". Lancet. 371 (9607): 143–52. doi:10.1016/S0140-6736(08)60107-5. PMID 18191686.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ Bachmann K, Mann O, Izbicki JR, Strate T (2008). "Chronic pancreatitis--a surgeons' view". Med. Sci. Monit. 14 (11): RA198–205. PMID 18971885.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ Nair RJ, Lawler L, Miller MR (2007). "Chronic pancreatitis". Am Fam Physician. 76 (11): 1679–88. PMID 18092710.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ Tattersall SJ, Apte MV, Wilson JS (2008). "A fire inside: current concepts in chronic pancreatitis". Intern Med J. 38 (7): 592–8. doi:10.1111/j.1445-5994.2008.01715.x. PMID 18715303.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ Hirvonen T, Pietinen P, Virtanen M, Albanes D, Virtamo J (15 July 1999). "Nutrient intake and use of beverages and the risk of kidney stones among male smokers". Am J Epidemiol. 150 (2): 187–94. PMID 10412964.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Soucie JM, Coates RJ, McClellan W, Austin H, Thun M (1 March 1996). "Relation between geographic variability in kidney stones prevalence and risk factors for stones". Am J Epidemiol. 143 (5): 487–95. PMID 8610664.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Curhan GC, Willett WC, Rimm EB, Spiegelman D, Stampfer MJ (1 February 1996). "Prospective study of beverage use and the risk of kidney stones". Am J Epidemiol. 143 (3): 240–7. PMID 8561157.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Curhan GC, Willett WC, Speizer FE, Stampfer MJ (1 April 1998). "Beverage use and risk for kidney stones in women". Ann Intern Med. 128 (7): 534–40. PMID 9518397.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Taniguchi N, Kaneko S (1997). "[Alcoholic effect on male sexual function]". Nippon Rinsho (in Japanese). 55 (11): 3040–4. PMID 9396310.
{{cite journal}}: Unknown parameter|month=ignored (help) - ^ Yoshitsugu M, Ihori M (1997). "[Endocrine disturbances in liver cirrhosis--focused on sex hormones]". Nippon Rinsho (in Japanese). 55 (11): 3002–6. PMID 9396303.
{{cite journal}}: Unknown parameter|month=ignored (help) - ^ Fentiman, IS.; Fourquet, A.; Hortobagyi, GN. (2006). "Male breast cancer". Lancet. 367 (9510): 595–604. doi:10.1016/S0140-6736(06)68226-3. PMID 16488803.
{{cite journal}}: Unknown parameter|month=ignored (help) - ^ Gavaler, JS. (1998). "Alcoholic beverages as a source of estrogens". Alcohol Health Res World. 22 (3): 220–7. PMID 15706799.
- ^ a b Weiss, JR.; Moysich, KB.; Swede, H. (2005). "Epidemiology of male breast cancer". Cancer Epidemiol Bio-markers Prev. 14 (1): 20–6. PMID 15668471.
{{cite journal}}: Unknown parameter|month=ignored (help) - ^ Boffetta, P.; Hashibe, M. (2006). "Alcohol and cancer". Lancet Oncol. 7 (2): 149–56. doi:10.1016/S1470-2045(06)70577-0. PMID 16455479.
{{cite journal}}: Unknown parameter|month=ignored (help) - ^ Carlsson S, Hammar N, Grill V, Kaprio J (2003). "Alcohol consumption and the incidence of type 2 diabetes: a 20-year follow-up of the Finnish twin cohort study". Diabetes Care. 26 (10): 2785–90. doi:10.2337/diacare.26.10.2785. PMID 14514580.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ J Hong1, R R Smith, A E Harvey and N P Núñez Alcohol consumption promotes insulin sensitivity without affecting body fat levels International Journal of Obesity (2009) 33, 197–203; doi:10.1038/ijo.2008.266
- ^ Star VL, Hochberg MC (1993). "Prevention and management of gout". Drugs. 45 (2): 212–22. doi:10.2165/00003495-199345020-00004. PMID 7681372.
{{cite journal}}: Unknown parameter|month=ignored (help) - ^ Eggebeen AT (2007). "Gout: an update". Am Fam Physician. 76 (6): 801–8. PMID 17910294.
{{cite journal}}: Unknown parameter|month=ignored (help) - ^ http://arc.org.uk/arthinfo/patpubs/6033/6033.asp
- ^ Myllykangas-Luosujärvi R, Aho K, Kautiainen H, Hakala M (2000). "Reduced incidence of alcohol related deaths in subjects with rheumatoid arthritis". Ann Rheum Dis. 59 (1): 75–6. doi:10.1136/ard.59.1.75. PMC 1752983. PMID 10627433.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ Nagata C, Fujita S, Iwata H; et al. (1995). "Systemic lupus erythematosus: a case-control epidemiologic study in Japan". Int J Dermatol. 34 (5): 333–7. doi:10.1111/j.1365-4362.1995.tb03614.x. PMID 7607794.
{{cite journal}}: Explicit use of et al. in:|author=(help); Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ Aho K, Heliövaara M (1993). "Alcohol, androgens and arthritis". Ann Rheum Dis. 52 (12): 897. doi:10.1136/ard.52.12.897-b. PMC 1005228. PMID 8311545.
{{cite journal}}: Unknown parameter|month=ignored (help) - ^ Hardy CJ, Palmer BP, Muir KR, Sutton AJ, Powell RJ (1998). "Smoking history, alcohol consumption, and systemic lupus erythematosus: a case-control study". Ann Rheum Dis. 57 (8): 451–5. doi:10.1136/ard.57.8.451. PMC 1752721. PMID 9797548.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ Källberg H, Jacobsen S, Bengtsson C; et al. (2008). "Alcohol consumption is associated with decreased risk of rheumatoid arthritis; Results from two Scandinavian case-control studies". Ann Rheum Dis. 68 (2): 222–7. doi:10.1136/ard.2007.086314. PMC 2937278. PMID 18535114.
{{cite journal}}: Explicit use of et al. in:|author=(help); Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ Jonsson IM, Verdrengh M, Brisslert M; et al. (2007). "Ethanol prevents development of destructive arthritis". Proc Natl Acad Sci USA. 104 (1): 258–63. doi:10.1073/pnas.0608620104. PMC 1765445. PMID 17185416.
{{cite journal}}: Explicit use of et al. in:|author=(help); Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ Myllykangas-Luosujärvi R, Aho K, Kautiainen H, Hakala M (2000). "Reduced incidence of alcohol related deaths in subjects with rheumatoid arthritis". Ann Rheum Dis. 59 (1): 75–6. doi:10.1136/ard.59.1.75. PMC 1752983. PMID 10627433.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ Voigt LF, Koepsell TD, Nelson JL, Dugowson CE, Daling JR (1994). "Smoking, obesity, alcohol consumption, and the risk of rheumatoid arthritis". Epidemiology. 5 (5): 525–32. PMID 7986867.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ Siris ES, Miller PD, Barrett-Connor E; et al. (2001). "Identification and fracture outcomes of undiagnosed low bone mineral density in postmenopausal women: results from the National Osteoporosis Risk Assessment". JAMA. 286 (22): 2815–22. doi:10.1001/jama.286.22.2815. PMID 11735756.
{{cite journal}}: Explicit use of et al. in:|author=(help); Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ Rapuri PB, Gallagher JC, Balhorn KE, Ryschon KL (1 November 2000). "Alcohol intake and bone metabolism in elderly women". Am. J. Clin. Nutr. 72 (5): 1206–13. PMID 11063451.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Holbrook TL, Barrett-Connor E (1993). "A prospective study of alcohol consumption and bone mineral density". BMJ. 306 (6891): 1506–9. doi:10.1136/bmj.306.6891.1506. PMC 1677960. PMID 8518677.
{{cite journal}}: Unknown parameter|month=ignored (help) - ^ a b Ronis, MJ.; Wands, JR.; Badger, TM.; de la Monte, SM.; Lang, CH.; Calissendorff, J. (2007). "Alcohol-induced disruption of endocrine signaling". Alcohol Clin Exp Res. 31 (8): 1269–85. doi:10.1111/j.1530-0277.2007.00436.x. PMID 17559547.
{{cite journal}}: Unknown parameter|month=ignored (help) - ^ Peer, KS.; Newsham, KR. (2005). "A case study on osteoporosis in a male athlete: looking beyond the usual suspects". Orthop Nurs. 24 (3): 193–9, quiz 200–1. PMID 15928528.
- ^ Kostović K, Lipozencić J (2004). "Skin diseases in alcoholics". Acta Dermatovenerol Croat. 12 (3): 181–90. PMID 15369644.
- ^ Abrar A. Qureshi; Patrick L. Dominguez; Hyon K. Choi; Jiali Han; Gary Curhan Alcohol Intake and Risk of Incident Psoriasis in US Women: A Prospective Study Arch Dermatology doi:10.1001/archdermatol.2010.204
- ^ Brenner H, Rothenbacher D, Bode G, Adler G (6 December 1997). "Relation of smoking and alcohol and coffee consumption to active Helicobacter pylori infection: cross sectional study". BMJ. 315 (7121): 1489–92. PMC 2127930. PMID 9420488.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Aldoori WH, Giovannucci EL, Stampfer MJ, Rimm EB, Wing AL, Willett WC (1997). "A prospective study of alcohol, smoking, caffeine, and the risk of duodenal ulcer in men". Epidemiology. 8 (4): 420–4. doi:10.1097/00001648-199707000-00012. PMID 9209857.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ Cohen S, Tyrrell DA, Russell MA, Jarvis MJ, Smith AP (1993). "Smoking, alcohol consumption, and susceptibility to the common cold". Am J Public Health. 83 (9): 1277–83. doi:10.2105/AJPH.83.9.1277. PMC 1694990. PMID 8363004.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ Takkouche B, Regueira-Méndez C, García-Closas R, Figueiras A, Gestal-Otero JJ, Hernán MA (2002). "Intake of wine, beer, and spirits and the risk of clinical common cold". Am J Epidemiol. 155 (9): 853–8. doi:10.1093/aje/155.9.853. PMID 11978590.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ IARC Monographs on the Evaluation of Carcinogenic Risks to Humans: Volume 44 Alcohol Drinking: Summary of Data Reported and Evaluation
- ^ National Toxicology Program Alcoholic Beverage Consumption: Known to be a human carcinogen First listed in the Ninth Report on Carcinogens (2000)(PDF)
- ^ Boffetta P, Hashibe M, La Vecchia C, Zatonski W, Rehm J (2006). "The burden of cancer attributable to alcohol drinking". International Journal of Cancer. 119 (4): 884–7. doi:10.1002/ijc.21903. PMID 16557583.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ BBC Drinking over recommended limit 'raises cancer risk' 8 April 2011
- ^ Madlen Schütze et al Alcohol attributable burden of incidence of cancer in eight European countries based on results from prospective cohort study BMJ 2011; 342:d1584 doi:10.1136/bmj.d1584
- ^ WCRF World Cancer Research Fund / American Institute for Cancer Research. Food, Nutrition, Physical Activity, and the Prevention of Cancer: a Global Perspective. Washington DC: AICR, 2007
- ^ Homann N, Stickel F, König IR; et al. (2006). "Alcohol dehydrogenase 1C*1 allele is a genetic marker for alcohol-associated cancer in heavy drinkers". International Journal of Cancer. 118 (8): 1998–2002. doi:10.1002/ijc.21583. PMID 16287084.
{{cite journal}}: Explicit use of et al. in:|author=(help)CS1 maint: multiple names: authors list (link) - ^ Nat Rev Cancer. 2007 Aug;7(8):599-612. Molecular mechanisms of alcohol-mediated carcinogenesis. Seitz HK, Stickel F. http://www.josorge.com/publications/Citations/JGH/001.pdf
- ^ Acetaldehyde-DNA Adducts: Implications for the Molecular Mechanism of Alcohol-Related Carcinogenesis Brooks P, Theruvathu J Cho CH, Purohit V (eds): Alcohol, Tobacco and Cancer. Basel, Karger, 2006, pp 78-94 (DOI: 10.1159/000095017) http://content.karger.com/ProdukteDB/produkte.asp?Doi=95017
- ^ Ulleland CN (1972). "The offspring of alcoholic mothers". Ann. N. Y. Acad. Sci. 197: 167–9. doi:10.1111/j.1749-6632.1972.tb28142.x. PMID 4504588.
{{cite journal}}: Unknown parameter|month=ignored (help) - ^ Abel EL, Sokol RJ (1987). "Incidence of foetal alcohol syndrome and economic impact of FAS-related anomalies". Drug Alcohol Depend. 19 (1): 51–70. doi:10.1016/0376-8716(87)90087-1. PMID 3545731.
{{cite journal}}: Unknown parameter|month=ignored (help) - ^ Harada K (1993). "Emotional condition in alcohol withdrawal acute psychosis". Seishin Shinkeigaku Zasshi. 95 (7): 523–9. PMID 8234534.
- ^ Benton, Sarah Allen (2009). Understanding the High-Functioning Alcoholic – Professional Views and Personal Insights. Greenwood Publishing Group. ISBN 978-0-313-35280-5.
- ^ Press release (June 28, 2007). "Researchers Identify Alcoholic Subtypes". National Institutes of Health – National Institute on Alcohol Abuse and Alcoholism. Retrieved February 18, 2012.
- ^ "Volume of World Beer Production". European Beer Guide. Archived from the original on 28 October 2006. Retrieved 17 October 2006.
{{cite web}}: Unknown parameter|deadurl=ignored (|url-status=suggested) (help) - ^ Nelson, Max (2005). The Barbarian's Beverage: A History of Beer in Ancient Europe. Abingdon, Oxon: Routledge. p. 1. ISBN 0-415-31121-7. Retrieved 21 September 2010.
- ^ Rudgley, Richard (1993). The Alchemy of Culture: Intoxicants in Society. London: British Museum Press. p. 411. ISBN 978-0-7141-1736-2. Retrieved 13 January 2012.
- ^ Arnold, John P (2005). Origin and History of Beer and Brewing: From Prehistoric Times to the Beginning of Brewing Science and Technology. Cleveland, Ohio: Reprint Edition by BeerBooks. p. 411. ISBN 0-9662084-1-2. Retrieved 13 January 2012.
- ^ Joshua J. Mark (2011). Beer. Ancient History Encyclopedia.
- ^ World's Best Beers: One Thousand. Google Books. 6 October 2009. ISBN 978-1-4027-6694-7. Retrieved 7 August 2010.
- ^ "About 37 percent of college students could now be considered alcoholics". Dailyemerald.com. 2012-05-22. Retrieved 2013-02-05.
- ^ “Gender differences in alcohol use and alcohol dependence or abuse: 2004 or 2005.” The NSDUH Report.Accessed June 22, 2012.
- ^ http://pubs.niaaa.nih.gov/publications/aa68/aa68.htm
- ^ a b Oscar-Berman M, Marinkovic K (2003). "Alcoholism and the brain: an overview". Alcohol Res Health. 27 (2): 125–33. PMID 15303622. Free full-text.
- ^ Liang, H.; Wang, Jianbing; Xiao, Huijuan; Wang, Ding; Wei, Wenqiang; Qiao, Youlin; Boffetta, Paolo (2010). "Estimation of cancer incidence and mortality attributable to alcohol drinking in China". BMC Public Health. 10 (1): 730. doi:10.1186/1471-2458-10-730.
{{cite journal}}: CS1 maint: unflagged free DOI (link) - ^ "Alcohol Consumption May Increase Pancreatic Cancer Risk". Medical News Today. 2009-03-04.
- ^ "Moderate Alcohol Consumption Increases Risk of Cancer in Women". 2009-03-10.
- ^ "Alcohol Consumption May Increase Pancreatic Cancer Risk". Medicalnewstoday.com. Retrieved 2010-02-11.
- ^ "Can alcohol be good for you?". Cancer Research UK.
- ^ http://www.kurzweilai.net/alcohol-may-boost-risk-of-cancer-for-asians
- ^ Silvia Balbo, Lei Meng, Robin L. Bliss, Joni A. Jensen, Dorothy K. Hatsukami, Stephen S. Hecht, Kinetics of DNA Adduct Formation in the Oral Cavity after Drinking Alcohol, Cancer Epidemiology, Biomarkers & Prevention, 2012, DOI: 10.1158/1055-9965.EPI-11-1175
- ^ "Alcohol 'major cause of dementia'". National Health Service. 2008-05-11.
- ^ Campbell, Denis (2009-05-10). "Binge drinking 'increases risk' of dementia". London: The Guardian. Retrieved 2010-04-07.
- ^ a b "Alcohol 'could reduce dementia risk'". BBC News. 2002-01-25.
- ^ http://health.usnews.com/health-conditions/diabetes/type-2-diabetes
- ^ Kanis JA; Johansson H; Johnell O; et al. (2005). "Alcohol intake as a risk factor for fracture". Osteoporosis international : a journal established as result of cooperation between the European Foundation for Osteoporosis and the National Osteoporosis Foundation of the USA. 16 (7): 737–42. doi:10.1007/s00198-004-1734-y. PMID 15455194.
{{cite journal}}: Unknown parameter|author-separator=ignored (help); Unknown parameter|month=ignored (help) - ^ a b UNC Bowles Center for Alcohol Studies. Alcoholism and Obesity: Overlapping Brain Pathways? Center Line. Vol 14, 2003.
- ^ Thiele et al. Overlapping Peptide Control of Alcohol Self-Administration and Feeding. Alcohol Clin Exp Res, Vol 28, No 2, 2004: pp 288–294.
- ^ Breslow et al. Drinking Patterns and Body Mass Index in Never Smokers: National Health Interview Survey, 1997–2001. Am J Epidemiol 2005;161:368–376.
- ^ Taffe 2010
- ^ Morris 2009
- ^ Bleich 2003
- ^ Blanco 2005
- ^ Leonard 1986
- ^ Lovinger 1989
- ^ Davis 1992
- ^ Bernier 2011
- ^ Takadera 1990
- ^ Jones 1973
- ^ Mitchell 1999
- ^ Gil-Mohapel 2010
- ^ Brocardo 2011
- ^ Bergamini 2004
- ^ Heaton 2000
- ^ Khantzian, E.J. (1997). The self-medication hypothesis of drug use disorders: A reconsideration and recent applications. Harvard Review of Psychiatry, 4, 231-244.
- ^ a b Khantzian, E.J. (2003). The self-medication hypothesis revisited: The dually diagnosed patient. Primary Psychiatry, 10, 47-48, 53-54.
- ^ Khantzian, E.J. (1999). Treating addiction as a human process. Northvale, NJ: Jason Aronson.
- ^ Sarah W. Book, M.D., and Carrie L. Randall, Ph.D. Social anxiety disorder and alcohol use. Alcohol Research and Health, 2002.
- ^ Professor C Heather Ashton (1987). "Benzodiazepine Withdrawal: Outcome in 50 Patients". British Journal of Addiction. 82: 655–671.
- ^ Michelini S (1996). "Long-term use of benzodiazepines: tolerance, dependence and clinical problems in anxiety and mood disorders". Pharmacopsychiatry. 29 (4): 127–34. doi:10.1055/s-2007-979558. PMID 8858711.
{{cite journal}}: Unknown parameter|coauthors=ignored (|author=suggested) (help); Unknown parameter|month=ignored (help) - ^ Wetterling T (2000). "Psychopathology of alcoholics during withdrawal and early abstinence". Eur Psychiatry. 15 (8): 483–8. doi:10.1016/S0924-9338(00)00519-8. PMID 11175926.
{{cite journal}}: Unknown parameter|coauthors=ignored (|author=suggested) (help); Unknown parameter|month=ignored (help) - ^ Cowley DS (Jan 1, 1992). "Alcohol abuse, substance abuse, and panic disorder". Am J Med. 92 (1A): 41S–8S. doi:10.1016/0002-9343(92)90136-Y. PMID 1346485.
- ^ Cosci F (2007). "Alcohol use disorders and panic disorder: a review of the evidence of a direct relationship". J Clin Psychiatry. 68 (6): 874–80. doi:10.4088/JCP.v68n0608. PMID 17592911.
{{cite journal}}: Unknown parameter|coauthors=ignored (|author=suggested) (help); Unknown parameter|month=ignored (help) - ^ a b Cohen SI (1995). "Alcohol and benzodiazepines generate anxiety, panic and phobias". J R Soc Med. 88 (2): 73–7. PMC 1295099. PMID 7769598.
{{cite journal}}: Unknown parameter|month=ignored (help) - ^ Perry, Lacy. (2004-10-12) HowStuffWorks "How Hangovers Work". Health.howstuffworks.com. Retrieved on 2011-11-20.
- ^ a b https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2768203/
- ^ Holahan, Charles J.; Schutte, Kathleen K.; Brennan, Penny L.; Holahan, Carole K.; Moos, Bernice S.; Moos, Rudolf H. (2010). "Late-Life Alcohol Consumption and 20-Year Mortality". Alcoholism: Clinical and Experimental Research. 34 (11): 1961–71. PMID 20735372.
- ^ a b "Alcohol may prevent diabetes". BBC News. 2002-05-15.
- ^ Dr Roger Henderson, GP (2006-01-17). "Alcohol and diabetes". Net Doctor.
- ^ a b Klatsky, A L; Friedman, G D (1995). "Alcohol and longevity". American Journal of Public Health. 85 (1): 16–8. doi:10.2105/AJPH.85.1.16. PMC 1615277. PMID 7832254.
- ^ a b Doll, R.; Peto, R; Boreham, J; Sutherland, I (2004). "Mortality in relation to alcohol consumption: a prospective study among male British doctors". International Journal of Epidemiology. 34 (1): 199–204. doi:10.1093/ije/dyh369. PMID 15647313.
- ^ "Frequent tipple cuts heart risk". BBC News. 2008-01-09.
- ^ "Alcohol and heart disease". British Heart Foundation.
- ^ "Moderate Drinking Lowers Women's Risk Of Heart Attack". Science Daily. 2007-05-25.
- ^ Rodgers, H; Aitken, PD; French, JM; Curless, RH; Bates, D; James, OF (1993). "Alcohol and stroke. A case-control study of drinking habits past and present". Stroke; a journal of cerebral circulation. 24 (10): 1473–7. PMID 8378949.



