History of medicine: Difference between revisions
→Renaissance to Early Modern period 16th-18th century: start on Bologna |
→Bibliography: add cites |
||
| Line 202: | Line 202: | ||
== Bibliography == |
== Bibliography == |
||
* Berridge, Virginia. "Health and Medicine" in ''The Cambridge Social History of Britain, 1750-1950, vol. 3, Social Agencies and Institutions,'' edited by F M.L. Thompson, (1990). |
* Berridge, Virginia. "Health and Medicine" in ''The Cambridge Social History of Britain, 1750-1950, vol. 3, Social Agencies and Institutions,'' edited by F M.L. Thompson, (1990). |
||
* Bynum, W. F. and Roy Porter, eds. ''Companion Encyclopedia of the History of Medicine'' (2 vol. 1997); 1840pp; 72 long essays by scholars [http://www.amazon.com/Companion-Encyclopedia-History-Medicine-Set/dp/0415164184/ excerpt and text search] |
|||
| ⚫ | |||
** Bynum, W.F. et al. ''The Western Medical Tradition: 1800-2000'' (2006) [http://www.amazon.com/Western-Medical-Tradition-1800-2000/dp/0521475651/ excerpt and text search] |
|||
* Conrad, Lawrence I. et al. '' The Western Medical Tradition: 800 BC to AD 1800'' (1995); [http://www.amazon.com/Western-Medical-Tradition-800-1800/dp/0521475643/ excerpt and text search] |
|||
* Loudon, Irvine, ed. ''Western Medicine: An Illustrated History'' (1997) [http://www.questia.com/read/97988313/western-medicine-an-illustrated-history online] |
|||
* McGrew, Roderick. ''Encyclopedia of Medical History'' (1985) |
|||
* {{cite book | title = The Greatest Benefit to Mankind: A Medical History of Humanity from Antiquity to the Present | last = [[Roy Porter|Porter]] | first = Roy | year = 1997 | publisher = Harper Collins | isbn = 0-00-215173-1 }} |
* {{cite book | title = The Greatest Benefit to Mankind: A Medical History of Humanity from Antiquity to the Present | last = [[Roy Porter|Porter]] | first = Roy | year = 1997 | publisher = Harper Collins | isbn = 0-00-215173-1 }} |
||
| ⚫ | |||
| ⚫ | |||
* Porter, Roy, ed. '' The Cambridge Illustrated History of Medicine'' (2001) [http://www.amazon.com/Cambridge-Illustrated-History-Medicine-Histories/dp/0521002524/ excerpt and text search] |
|||
| ⚫ | |||
** Porter, Roy, ed. '' The Cambridge History of Medicine'' (2006); 416pp; [http://www.amazon.com/Cambridge-History-Medicine-Roy-Porter/dp/0521682894/ excerpt and text search] same text without the illustrations |
|||
| ⚫ | |||
* Porter, Roy. '' Blood and Guts: A Short History of Medicine'' (2004) 224pp; [http://www.amazon.com/Blood-Guts-Short-History-Medicine/dp/0393325695/ excerpt and text search] |
|||
| ⚫ | |||
| ⚫ | |||
* Singer, Charles, and E. Ashworth Underwood. ''A Short History of Medicine'' (2nd ed. 1962) |
|||
| ⚫ | |||
* Siraisi, Nancy G. '' Medieval and Early Renaissance Medicine: An Introduction to Knowledge and Practice'' (1990) [http://www.amazon.com/Medieval-Early-Renaissance-Medicine-Introduction/dp/0226761304/ excerpt and text search] |
|||
* Warner, John Harley, and Janet A. Tighe, eds. ''Major Problems in the History of American Medicine and Public Health'' (2006), 560pp; readings in primary and secondary sources [http://www.amazon.com/gp/reader/0395954355/ excerpt and text search] |
* Warner, John Harley, and Janet A. Tighe, eds. ''Major Problems in the History of American Medicine and Public Health'' (2006), 560pp; readings in primary and secondary sources [http://www.amazon.com/gp/reader/0395954355/ excerpt and text search] |
||
* Watts, Sheldon. ''Disease and Medicine in World History'' (2003), 166pp [http://www.questia.com/read/107990563/disease-and-medicine-in-world-history online] |
|||
* Weatherall, Miles. ''In Search of a Cure: A History of Pharmaceutical Discovery'' (1990), emphasis on antibiotics. |
* Weatherall, Miles. ''In Search of a Cure: A History of Pharmaceutical Discovery'' (1990), emphasis on antibiotics. |
||
* Wohl, Anthony S. ''Endangered Lives: Public Health in Victorian Britain'' (1983). |
* Wohl, Anthony S. ''Endangered Lives: Public Health in Victorian Britain'' (1983). |
||
=== Primary sources === |
|||
| ⚫ | |||
| ⚫ | |||
== External links == |
== External links == |
||
Revision as of 15:54, 20 February 2013
Template:History of science sidebar
All human societies have medical beliefs that provide explanations for birth, death, and disease. Throughout history, illness has been attributed to witchcraft, demons, astral influence, or the will of the gods. These ideas still retain some power, with faith healing and shrines still used in some places, although the rise of scientific medicine over the past millennium has altered or replaced mysticism in most cases.
The ancient Egyptians had a system of medicine that was very advanced for its time and influenced later medical traditions. The Egyptians and Babylonians both introduced the concepts of diagnosis, prognosis, and medical examination. The Hippocratic Oath, still taken by doctors today, was written in Greece in the 5th century BCE. In the medieval era, surgical practices inherited from the ancient masters were improved and then systematized in Rogerius's The Practice of Surgery. During the Renaissance, understanding of anatomy improved, and the invention of the microscope would later lead to the germ theory of disease. These advancements, along with developments in chemistry, genetics, and lab technology (such as the x-ray) led to modern medicine.
Prehistoric medicine
Although there is no record to establish when plants were first used for medicinal purposes (herbalism), the use of plants as healing agents is a long-standing practice. Over time through emulation of the behavior of fauna a medicinal knowledge base developed and was passed between generations. As tribal culture specialized specific castes, Shamans and apothecaries performed the 'niche occupation' of healing.
Antiquity
Egypt
Ancient Egypt developed a large, varied and fruitful medical tradition. Herodotus described the Egyptians as "the healthiest of all men, next to the Libyans",[1] due to the dry climate and the notable public health system that they possessed. According to him, "[t]he practice of medicine is so specialized among them that each physician is a healer of one disease and no more." Although Egyptian medicine, to a good extent, dealt with the supernatural,[2] it eventually developed a practical use in the fields of anatomy, public health, and clinical diagnostics.
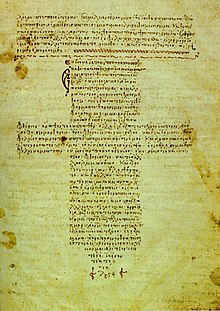
Medical information in the Edwin Smith Papyrus[3] may date to a time as early as 3000 BCE.[4] The earliest known surgery was performed in Egypt around 2750 BCE. Imhotep in the 3rd dynasty is sometimes credited with being the founder of ancient Egyptian medicine and with being the original author of the Edwin Smith Papyrus, detailing cures, ailments and anatomical observations. The Edwin Smith Papyrus is regarded as a copy of several earlier works and was written c. 1600 BCE. It is an ancient textbook on surgery almost completely devoid of magical thinking and describes in exquisite detail the examination, diagnosis, treatment, and prognosis of numerous ailments.[5]
Conversely, the Ebers papyrus[6] (c. 1550 BCE) is full of incantations and foul applications meant to turn away disease-causing demons, and other superstition. The Ebers papyrus also provides our earliest possible documentation of ancient awareness of tumors, but ancient medical terminology being badly understood, cases Ebers 546 and 547[vague] for instance may refer to simple swellings.
The Kahun Gynaecological Papyrus[7] treats women's complaints, including problems with conception. Thirty four cases detailing diagnosis and treatment survive, some of them fragmentarily.[8] Dating to 1800 BCE, it is the oldest surviving medical text of any kind.
Medical institutions, referred to as Houses of Life are known to have been established in ancient Egypt as early as the 1st Dynasty.[citation needed]
The earliest known physician is also credited to ancient Egypt: Hesy-Ra, “Chief of Dentists and Physicians” for King Djoser in the 27th century BCE.[9] Also, the earliest known woman physician, Peseshet, practiced in Ancient Egypt at the time of the 4th dynasty. Her title was “Lady Overseer of the Lady Physicians.” In addition to her supervisory role, Peseshet trained midwives at an ancient Egyptian medical school in Sais.[citation needed]
Mesopotamia and Levant
The oldest Babylonian texts on medicine date back to the Old Babylonian period in the first half of the 2nd millennium BCE. The most extensive Babylonian medical text, however, is the Diagnostic Handbook written by the ummânū, or chief scholar, Esagil-kin-apli of Borsippa,[10] during the reign of the Babylonian king Adad-apla-iddina (1069-1046 BCE).[11]
Along with contemporary ancient Egyptian medicine, the Babylonians introduced the concepts of diagnosis, prognosis, physical examination, and medical prescriptions. In addition, the Diagnostic Handbook introduced the methods of therapy and etiology and the use of empiricism, logic and rationality in diagnosis, prognosis and therapy. The text contains a list of medical symptoms and often detailed empirical observations along with logical rules used in combining observed symptoms on the body of a patient with its diagnosis and prognosis.[12]
The Diagnostic Handbook was based on a logical set of axioms and assumptions, including the modern view that through the examination and inspection of the symptoms of a patient, it is possible to determine the patient's disease, its aetiology and future development, and the chances of the patient's recovery. The symptoms and diseases of a patient were treated through therapeutic means such as bandages, creams and pills.[10]
Most of our knowledge of ancient Hebrew medicine during the 1st millennium BCE comes from the Torah, i.e. the Five Books of Moses, which contain various health related laws and rituals, such as isolating infected people (Leviticus 13:45-46), washing after handling a dead body (Numbers 19:11-19) and burying excrement away from camp (Deuteronomy 23:12-13). While the observance of these statutes would have and do lead to several health benefits, Jewish belief commands that these rituals and prohibitions be kept purely to fulfill the will of God with no ulterior motive. Max Neuberger, writing in his "History of Medicine" says
- "The commands concern prophylaxis and suppression of epidemics, suppression of venereal disease and prostitution, care of the skin, baths, food, housing and clothing, regulation of labour, sexual life, discipline of the people, etc. Many of these commands, such as Sabbath rest, circumcision, laws concerning food (interdiction of blood and pork), measures concerning menstruating and lying-in women and those suffering from gonorrhea, isolation of lepers, and hygiene of the camp, are, in view of the conditions of the climate, surprisingly rational." (Neuburger: History of Medicine, Oxford University Press, 1910, Vol. I, p. 38).
India
The Atharvaveda, a sacred text of Hinduism dating from the Early Iron Age, is the first Indian text dealing with medicine, like the medicine of the Ancient Near East based on concepts of the exorcism of demons and magic. The Atharvaveda also contain prescriptions of herbs for various ailments. The use of herbs to treat ailments would later form a large part of Ayurveda.
In the first millennium BCE, there emerges in post-Vedic India the traditional medicine system known as Ayurveda, meaning the "complete knowledge for long life". Its two most famous texts belong to the schools of Charaka, born c. 600 BCE, and Sushruta, born 600 BCE. While these writings display some limited continuities with the earlier medical ideas known from the Vedas, historians[who?] have been able to demonstrate direct historical connections between early Ayurveda and the early literature of the Buddhists and Jains. The earliest foundations of Ayurveda were built on a synthesis of traditional herbal practices together with a massive addition of theoretical conceptualizations, new nosologies and new therapies dating from about 400 BCE onwards, and coming out of the communities of thinkers who included the Buddha and others.[13]
According to the compendium of Charaka, the Charakasamhitā, health and disease are not predetermined and life may be prolonged by human effort. The compendium of Suśruta, the Suśrutasamhitā defines the purpose of medicine to cure the diseases of the sick, protect the healthy, and to prolong life. Both these ancient compendia include details of the examination, diagnosis, treatment, and prognosis of numerous ailments. The Suśrutasamhitā is notable for describing procedures on various forms of surgery, including rhinoplasty, the repair of torn ear lobes, perineal lithotomy, cataract surgery, and several other excisions and other surgical procedures. Most remarkable is Sushruta's penchant for scientific classification: His medical treatise consists of 184 chapters, 1,120 conditions are listed, including injuries and illnesses relating to ageing and mental illness. The Sushruta Samhita describe 125 surgical instrument, 300 surgical procedures and classifies human surgery in 8 categories [14]
The Ayurvedic classics mention eight branches of medicine: kāyācikitsā (internal medicine), śalyacikitsā (surgery including anatomy), śālākyacikitsā (eye, ear, nose, and throat diseases), kaumārabhṛtya (pediatrics), bhūtavidyā (spirit medicine), and agada tantra (toxicology), rasāyana (science of rejuvenation), and vājīkaraṇa (aphrodisiacs, mainly for men). Apart from learning these, the student of Āyurveda was expected to know ten arts that were indispensable in the preparation and application of his medicines: distillation, operative skills, cooking, horticulture, metallurgy, sugar manufacture, pharmacy, analysis and separation of minerals, compounding of metals, and preparation of alkalis. The teaching of various subjects was done during the instruction of relevant clinical subjects. For example, teaching of anatomy was a part of the teaching of surgery, embryology was a part of training in pediatrics and obstetrics, and the knowledge of physiology and pathology was interwoven in the teaching of all the clinical disciplines. The normal length of the student's training appears to have been seven years. But the physician was to continue to learn.[15]
As an alternative form of medicine in India, Unani medicine got deep roots and royal patronage during medieval times. It progressed during Indian sultanate and mughal periods. Unani medicine is very close to Ayurveda. Both are based on theory of the presence of the elements (in Unani, they are considered to be fire, water, earth and air) in the human body. According to followers of Unani medicine, these elements are present in different fluids and their balance leads to health and their imbalance leads to illness.[16]
China
China also developed a large body of traditional medicine. Much of the philosophy of traditional Chinese medicine derived from empirical observations of disease and illness by Taoist physicians and reflects the classical Chinese belief that individual human experiences express causative principles effective in the environment at all scales. These causative principles, whether material, essential, or mystical, correlate as the expression of the natural order of the universe.
The foundational text of Chinese medicine is the Huangdi neijing, or Yellow Emperor's Inner Canon, which is composed of two books: the Suwen 素問 ("Basic Questions") and the Lingshu 靈樞 ("Divine Pivot"). Although the Neijing has long been attributed to the mythical Yellow Emperor (twenty-7th century BCE), Chinese scholars started doubting this attribution as early as the 11th century and now usually date the Neijing to the late Warring States period (5th century-221 BCE).[17] Because the medical "silk manuscripts" dating from around 200 BCE that were excavated in the 1970s from the tomb of a Han-dynasty noble in Mawangdui are undoubtedly ancestors of the received Neijing, scholars like Nathan Sivin now argue that the Neijing was first compiled in the 1st century BCE.[18]
During the Han dynasty, Zhang Zhongjing, who was mayor of Changsha near the end of the 2nd century AD, wrote a Treatise on Cold Damage, which contains the earliest known reference to the Neijing Suwen. The Jin Dynasty practitioner and advocate of acupuncture and moxibustion, Huangfu Mi (215-282), also quotes the Yellow Emperor in his Jiayi jing, c. 265. During the Tang Dynasty, Wang Bing claimed to have located a copy of the originals of the Suwen, which he expanded and edited substantially. This work was revisited by an imperial commission during the 11th century, and the result is our best extant representation of the foundational roots of traditional Chinese medicine.
Traditional Chinese Medicine that is based on the use of herbal medicine, acupuncture, massage and other forms of therapy has been practiced in China for thousands of years. However, Western Medicine was introduced to China in the 19th Century, mainly by medical missionaries sent from various Christian mission organizations, such as the London Missionary Society (Britain), the Methodist Church (Britain) and the Presbyterian Church (USA). Benjamin Hobson (1816-1873), a medical missionary sent by the London Missionary Society in 1839, set up a highly successful Wai Ai Clinic (惠愛醫館) [19][20] in Guangzhou, China. The Hong Kong College of Medicine for Chinese (香港華人西醫書院) was founded in 1887 by the London Missionary Society, with its first graduate (in 1892) being Sun Yat-sen (孫中山). Sun later led the Chinese Revolution (1911), which changed China from an empire to a republic. The Hong Kong College of Medicine for Chinese was the forerunner of the School of Medicine of the University of Hong Kong, which started in 1911.
Due to the social custom that men and women should not be near to one another, the women of China were reluctant to be treated by male doctors of Western Medicine. This resulted in a tremendous need for female doctors of Western Medicine in China. Thus, female medical missionary Dr. Mary H. Fulton (1854-1927) [21] was sent by the Foreign Missions Board of the Presbyterian Church (USA) to found the first medical college for women in China. Known as the Hackett Medical College for Women (夏葛女子醫學院),[22][23] this College was located in Guangzhou, China, and was enabled by a large donation from Mr. Edward A.K. Hackett (1851-1916) of Indiana, USA. The College was dedicated in 1902 and offered a four-year curriculum. By 1915, there were more than 60 students, mostly in residence. Most students became Christians, due to the influence of Dr. Fulton. The College was officially recognized, with its diplomas marked with the official stamp of the Guangdong provincial government. The College was aimed at the spreading of Christianity and modern medicine and the elevation of Chinese women's social status. The David Gregg Hospital for Women and Children (also known as Yuji Hospital 柔濟醫院) [24][25] was affiliated with this College. The graduates of this College included CHAU Lee-sun (周理信, 1890-1979) and WONG Yuen-hing (黃婉卿), both of whom graduated in the late 1910s [26][27] and then practiced medicine in the hospitals in Guangdong province.
Greek and Roman medicine
Homer
Around 800 BCE Homer in The Iliad gives descriptions of wound treatment by "the two sons of Asklepios, the admirable physicians Podaleirius and Machaon and one acting doctor, Patroclus. Because Machaon is wounded and Podaleirius is in combat Eurypylus asks Patroclus “to cut out this arrow from my thigh, wash off the blood with warm water and spread soothing ointment on the wound." Askelpios like Imhotep becomes god of healing over time. Temples dedicated to the healer-god Asclepius, known as Asclepieia (Ancient Greek: Ἀσκληπιεῖα, sing. Ἀσκληπιεῖον, 'Asclepieion), functioned as centers of medical advice, prognosis, and healing.[28] At these shrines, patients would enter a dream-like state of induced sleep known as enkoimesis (ἐγκοίμησις) not unlike anesthesia, in which they either received guidance from the deity in a dream or were cured by surgery.[29] Asclepeia provided carefully controlled spaces conducive to healing and fulfilled several of the requirements of institutions created for healing.[28] In the Asclepieion of Epidaurus, three large marble boards dated to 350 BCE preserve the names, case histories, complaints, and cures of about 70 patients who came to the temple with a problem and shed it there. Some of the surgical cures listed, such as the opening of an abdominal abscess or the removal of traumatic foreign material, are realistic enough to have taken place, but with the patient in a state of enkoimesis induced with the help of soporific substances such as opium.[29]
The first known Greek medical school opened in Cnidus in 700 BCE. Alcmaeon, author of the first anatomical work, worked at this school, and it was here that the practice of observing patients was established. As was the case elsewhere, the ancient Greeks developed a humoral medicine system where treatment sought to restore the balance of humours within the body.
Hippocrates
A towering figure in the history of medicine was the physician Hippocrates of Kos (c. 460 – c. 370 BCE), considered the "father of modern medicine."[30][31] The Hippocratic Corpus is a collection of around seventy early medical works from ancient Greece strongly associated with Hippocrates and his students. Most famously, Hippocrates invented the Hippocratic Oath for physicians, which is still relevant and in use today.
Hippocrates and his followers were first to describe many diseases and medical conditions. He is given credit for the first description of clubbing of the fingers, an important diagnostic sign in chronic suppurative lung disease, lung cancer and cyanotic heart disease. For this reason, clubbed fingers are sometimes referred to as "Hippocratic fingers".[citation needed] Hippocrates was also the first physician to describe Hippocratic face in Prognosis. Shakespeare famously alludes to this description when writing of Falstaff's death in Act II, Scene iii. of Henry V.[citation needed]
Hippocrates began to categorize illnesses as acute, chronic, endemic and epidemic, and use terms such as, "exacerbation, relapse, resolution, crisis, paroxysm, peak, and convalescence."[32][33][34]
Another of Hippocrates's major contributions may be found in his descriptions of the symptomatology, physical findings, surgical treatment and prognosis of thoracic empyema, i.e. suppuration of the lining of the chest cavity. His teachings remain relevant to present-day students of pulmonary medicine and surgery. Hippocrates was the first documented chest surgeon and his findings are still valid.


Celsus and Alexandria
Two great Alexandrians laid the foundations for the scientific study of anatomy and physiology, Herophilus of Chalcedon and Erasistratus of Ceos.[36] Other Alexandrian surgeons gave us; ligature (hemostasis), lithotomy, hernia operations, ophthalmic surgery, plastic surgery, methods of reduction of dislocations and fractures,tracheotomy, and mandrake as anesthesia. Most of what we know of them comes from Celsus and Galen of Pergamum (Greek: Γαληνός)[37]
Herophilus of Chalcedon, working at the medical school of Alexandria placed intelligence in the brain, and connected the nervous system to motion and sensation. Herophilus also distinguished between veins and arteries, noting that the latter pulse while the former do not. He and his contemporary, Erasistratus of Chios, researched the role of veins and nerves, mapping their courses across the body. Erasistratus connected the increased complexity of the surface of the human brain compared to other animals to its superior intelligence. He sometimes employed experiments to further his research, at one time repeatedly weighing a caged bird, and noting its weight loss between feeding times. In Erasistratus' physiology, air enters the body, is then drawn by the lungs into the heart, where it is transformed into vital spirit, and is then pumped by the arteries throughout the body. Some of this vital spirit reaches the brain, where it is transformed into animal spirit, which is then distributed by the nerves.[38]
Galen
The Greek Galen was one of the greatest surgeons of the ancient world and performed many audacious operations—including brain and eye surgeries— that were not tried again for almost two millennia. Later, in medieval Europe, Galen's writings on anatomy became the mainstay of the medieval physician's university curriculum along; but they suffered greatly from stasis and intellectual stagnation. In the 1530s, however, Belgian anatomist and physician Andreas Vesalius took on a project to translate many of Galen's Greek texts into Latin. Vesalius's most famous work, De humani corporis fabrica, was greatly influenced by Galenic writing and form.[39] The works of Galen were regarded as authoritative until well into the Middle Ages.
The Romans invented numerous surgical instruments, including the first instruments unique to women,[40] as well as the surgical uses of forceps, scalpels, cautery, cross-bladed scissors, the surgical needle, the sound, and speculas.[41][42] Romans also performed cataract surgery.[43]
Islamic Middle Ages 9th-12th

The Islamic civilization rose to primacy in medical science as its physicians contributed significantly to the field of medicine, including anatomy, ophthalmology, pharmacology, pharmacy, physiology, surgery, and the pharmaceutical sciences. The Arabs were influenced by, and further developed Greek, Roman and Byzantine medical practices. Galen, Hippocrates, were pre-eminent authorities.The translation of 129 works of ancient Greek physician Galen into Arabic by Hunayn ibn Ishaq and his assistants, and in particular Galen's insistence on a rational systematic approach to medicine, set the template for Islamic medicine, which rapidly spread throughout the Arab Empire. Muslim physicians set up dedicated hospitals,[44][verification needed]
Scholastic Medicine 13th-16th century
In western Europe, with the collapse of Roman imperial authority, medicine became localised; folk-medicine supplemented what remained of the medical knowledge of antiquity. Medical knowledge was preserved and practised in many monastic institutions, which often had a hospital attached. Organised professional medicine re-emerged, with the foundation of the medical college (Schola Medica Salernitana) of Salerno in Italy in the 11th century, which in co-operation with the monastery of Monte Cassino, translated many Byzantine and Arabic works. In the 12th century universities were founded in Italy and elsewhere, which soon developed schools of medicine. By the 13th century, many European towns were demanding that physicians have several years of study or training before they could practice. Montpellier, Padua and Bologna Universities were particularly interested in the academic side to medicine, and by the 15th century at the latest, Surgery was a separate university subject to Physic (Medicine).
Renaissance to Early Modern period 16th-18th century
The Renaissance brought an intense focus on scholarship to Christian Europe. A major effort to translate the Arabic and Greek scientific works into Latin emerged. Europeans gradually became experts not only the ancient writings of the Romans and Greeks, but in the contemporary writings of Islamic scientists. During the later centuries of the Renaissance came an increase in experimental investigation, particularly in the field of dissection and body examination, thus advancing our knowledge of human anatomy.[45] The development of modern neurology began in the 16th century with Vesalius, who described the anatomy of the brain and other organs; he had little knowledge of the brain's function, thinking that it resided mainly in the ventricles. Over his lifetime he corrected over 200 of Galen's mistakes. Understanding of medical sciences and diagnosis improved, but with little direct benefit to health care. Few effective drugs existed, beyond opium and quinine. Folklore cures and potentially poisonous metal-based compounds were popular treatments. Independently from Ibn al-Nafis, Michael Servetus rediscovered the pulmonary circulation, but this discovery did not reach the public cause it was written down for the first time in the "Manuscript of Paris"[46] in 1546, and later published in the theological work which he paid with his life in 1553. Later this was perfected by Renaldus Columbus and Andrea Cesalpino. Later William Harvey provided a refined and complete description of the circulatory system. The most useful tomes in medicine used both by students and expert physicians were Materia Medica and Pharmacopoeia.
Bologna
At the University of Bologna the training of physicians began in 1219. The Italian city attracted students from across Europe. Taddeo Alderotti built a tradition of medical education that established the characteristic features of Italian learned medicine and was copied by medical schools elsewhere.[47]
19th century: Rise of modern medicine

The practice of medicine changed in the face of rapid advances in science, as well as new approaches by physicians. Hospital doctors began much more systematic analysis of patients' symptoms in diagnosis.[48] Among the more powerful new techniques were anaesthesia, and the development of both antiseptic and aseptic operating theatres.[49] Actual cures were developed for certain endemic infectious diseases. However the decline in many of the most lethal diseases was more due to improvements in public health and nutrition than to medicine. It was not until the 20th century that the application of the scientific method to medical research began to produce multiple important developments in medicine, with great advances in pharmacology and surgery.
Medicine was revolutionized in the 19th century and beyond by advances in chemistry and laboratory techniques and equipment, old ideas of infectious disease epidemiology were replaced with bacteriology and virology. Bacteria and microorganisms were first observed with a microscope by Antonie van Leeuwenhoek in 1676, initiating the scientific field microbiology.[50]
Ignaz Semmelweis (1818–1865) in 1847 dramatically reduced the death rate of new mothers from childbed fever by the simple expedient of requiring physicians to clean their hands before attending to women in childbirth. His discovery pre-dated the germ theory of disease. However, his discoveries were not appreciated by his contemporaries and came into general use only with discoveries of British surgeon Joseph Lister, who in 1865 proved the principles of antisepsis in the treatment of wounds; However, medical conservatism on new breakthroughs in pre-existing science prevented them from being generally well received during the 19th century. Semmelweis's work was supported by the discoveries made by Louis Pasteur. Linking microorganisms with disease, Pasteur brought about a revolution in medicine. He also invented with Claude Bernard (1813–1878) the process of pasteurization still in use today. His experiments confirmed the germ theory. Claude Bernard aimed at establishing scientific method in medicine; he published An Introduction to the Study of Experimental Medicine in 1865. Beside this, Pasteur, along with Robert Koch (who was awarded the Nobel Prize in 1905), founded bacteriology. Koch was also famous for the discovery of the tubercle bacillus (1882) and the cholera bacillus (1883) and for his development of Koch's postulates.
The participation of women in medical care (beyond serving as midwives, sitters and cleaning women) was brought about by Florence Nightingale. Nightingale showed a previously male dominated profession the elemental role of nursing in order to lessen the aggravation of patient mortality which resulted from lack of hygiene and nutrition. Nightingale set up the St Thomas hospital, post-Crimea, in 1852. The International Red Cross began operations in numerous countries in the late 19th century, promoting nursing as an ideal profession for middle class women.[51]
Elizabeth Blackwell (1821–1910) became the first woman to formally study, and subsequently practice, medicine in the United States.
Paris
In 1770s-1850s Paris became a world center of medical research and teaching. The "Paris School" emphasized that teaching and research should be based in large hospitals and promoted the professionalization of the medical profession and the emphasis on sanitation and public health. A major reformer was Jean-Antoine Chaptal (1756-1832), a physician who was Minister of Internal Affairs. He created the Paris Hospital, health councils, and other bodies.[52]
U.S. Civil War
In the American Civil War (1861–65), as was typical of the 19th century, more soldiers died of disease than in battle, and even larger numbers were temporarily incapacitated by wounds, disease and accidents.[53] Conditions were poor in the Confederacy, where doctors and medical supplies were in short supply.[54] The war had a dramatic long-term impact on American medicine, from surgerical technique to hospitals to nursing and to research facilities.
The hygiene of the training and field camps was poor, especially at the beginning of the war when men who had seldom been far from home were brought together for training with thousands of strangers. First came epidemics of the childhood diseases of chicken pox, mumps, whooping cough, and, especially, measles. Operations in the South meant a dangerous and new disease environment, bringing diarrhea, dysentery, typhoid fever, and malaria. There were no antibiotics, so the surgeons prescribed coffee, whiskey, and quinine. Harsh weather, bad water, inadequate shelter in winter quarters, poor policing of camps, and dirty camp hospitals took their toll.[55]
This was a common scenario in wars from time immemorial, and conditions faced by the Confederate army were even worse. The Union responded by building army hospitals in every state. What was different in the Union was the emergence of skilled, well-funded medical organizers who took proactive action, especially in the much enlarged United States Army Medical Department,[56] and the United States Sanitary Commission, a new private agency.[57] Numerous other new agencies also targeted the medical and morale needs of soldiers, including the United States Christian Commission as well as smaller private agencies such as the Women's Central Association of Relief for Sick and Wounded in the Army (WCAR) founded in 1861 by Henry Whitney Bellows, and Dorothea Dix. Systematic funding appeals raised public consciousness, as well as millions of dollars. Many thousands of volunteers worked in the hospitals and rest homes, most famously poet Walt Whitman. Frederick Law Olmstead, a famous landscape architect, was the highly efficient executive director of the Sanitary Commission.[58]
States could use their own tax money to support their troops as Ohio did. Following the unexpected carnage at the battle of Shiloh in April 1862, the Ohio state government sent 3 steamboats to the scene as floating hospitals with doctors, nurses and medical supplies. The state fleet expanded to eleven hospital ships. The state also set up 12 local offices in main transportation nodes to help Ohio soldiers moving back and forth.[59] The U.S. Army learned many lessons and in 1886, it established the Hospital Corps. The Sanitary Commission collected enormous amounts of statistical data, and opened up the problems of storing information for fast access and mechanically searching for data patterns. The pioneer was John Shaw Billings (1838-1913). A senior surgeon in the war, Billings built the Library of the Surgeon General's Office (now the National Library of Medicine, the centerpiece of modern medical information systems.[60] Billings figured out how to mechanically analyze medical and demographic data by turning it into numbers and punching onto cardboard cards as developed by his assistant Herman Hollerith, the origin of the computer punch card system that dominated statistical data manipulation until the 1970s.[61]
World Wars

The 20th century witnessed a shift from a master-apprentice paradigm of teaching of clinical medicine to a more "democratic" system of medical schools. With the advent of the evidence-based medicine and great advances of information technology the process of change is likely to evolve further, with greater development of international projects such as the Human genome project.
The ABO blood group system was discovered in 1901, and the Rhesus group in 1937, facilitating blood transfusion.
During the 20th century, large-scale wars were attended with medics and mobile hospital units which developed advanced techniques for healing massive injuries and controlling infections rampant in battlefield conditions. Thousands of scarred troops provided the need for improved prosthetic limbs and expanded techniques in plastic surgery or reconstructive surgery. Those practices were combined to broaden cosmetic surgery and other forms of elective surgery.
During the First World War, Alexis Carrel and Henry Dakin developed the Carrel-Dakin method of treating wounds with an irrigation, Dakin's solution, a germicide which helped prevent gangrene.
The Great War spurred the usage of Roentgen's X-ray, and the electrocardiograph, for the monitoring of internal bodily functions. This was followed in the inter-war period by the development of the first anti-bacterial agents such as the sulpha antibiotics. The Second World War saw the introduction of widespread and effective antimicrobial therapy with the development and mass production of penicillin antibiotics, made possible by the pressures of the war and the collaboration of British scientists with the American pharmaceutical industry.
The 1918 flu pandemic killed at least 50 million people around the world, and has become an important case study in epidemiology, see Spanish flu research.
Human subject research, and killing of patients with disabilities, were at its height during the mid-20th century, with Nazi human experimentation and Aktion T4 during the Holocaust as the most significant example, followed up by the Doctors' Trial. Principles of medical ethics, such as the Nuremberg Code, have been introduced to prevent atrocities.
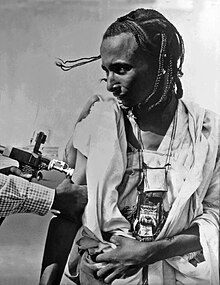
During and just after World War II, DDT was used as insecticide to combat insect vectors carrying malaria and typhus.
Psychiatric reform
Lunatic asylums began to appear in the Industrial Era. Emil Kraepelin (1856–1926) introduced new medical categories of mental illness, which eventually came into psychiatric usage despite their basis in behavior rather than pathology or etiology. In the 1920s surrealist opposition to psychiatry was expressed in a number of surrealist publications. In the 1930s several controversial medical practices were introduced including inducing seizures (by electroshock, insulin or other drugs) or cutting parts of the brain apart (leucotomy or lobotomy). Both came into widespread use by psychiatry, but there were grave concerns and much opposition on grounds of basic morality, harmful effects, or misuse. In the 1950s new psychiatric drugs, notably the antipsychotic chlorpromazine, were designed in laboratories and slowly came into preferred use. Although often accepted as an advance in some ways, there was some opposition, due to serious adverse effects such as tardive dyskinesia. Patients often opposed psychiatry and refused or stopped taking the drugs when not subject to psychiatric control. There was also increasing opposition to the use of psychiatric hospitals, and attempts to move people back into the community on a collaborative user-led group approach ("therapeutic communities") not controlled by psychiatry. Campaigns against masturbation were done in the Victorian era and elsewhere. Lobotomy was used until the 1970s to treat schizophrenia. This was denounced by the anti-psychiatric movement in the 1960s and later.
Post-World War II


The World Health Organization was founded in 1948 as a United Nations agency to improve global health. In most of the world, life expectancy has improved since then, and was about 67 years as of 2010, and well above 80 years in some countries. Eradication of infectious diseases is an international effort, and several new vaccines have been developed during the post-war years, against infections such as measles, mumps, several strains of influenza and human papilloma virus. The long-known vaccine against Smallpox finally eradicated the disease in the 1970s, and Rinderpest was wiped out in 2011. Eradication of polio is underway. Tissue culture is important for development of vaccines. Though the early success of antiviral vaccines and antibacterial drugs, antiviral drugs were not introduced until the 1970s. Through the WHO, the international community has developed a response protocol against epidemics, displayed during the SARS epidemic in 2003, and the Influenza A virus subtype H5N1 from 2004 and onwards.
As infectious diseases have become less lethal, and the most common causes of death in developed countries are now tumors and cardiovascular diseases, these conditions have received increased attention in medical research. Tobacco smoking as a cause of lung cancer was first researched in the 1920s, but was not widely supported by publications until the 1950s. Cancer treatment has been developed with radiotherapy and chemotherapy.
Oral rehydration therapy has been extensively used since the 1970s to treat cholera and other diarrhea-inducing infections.
Hormonal contraception was introduced in the 1950s, and was associated with the sexual revolution, with normalization of abortion and homosexuality in many countries. Family planning has promoted a demographic transition in most of the world. With threatening sexually transmitted infections, not least HIV, use of barrier contraception has become imperative. The struggle against HIV has provided no cure, but improved antiretroviral treatments, and in the late 2000s (decade), male circumcision was proved to diminish infection risk.[citation needed]
X-ray imaging was the first kind of medical imaging, and later ultrasonic imaging, CT scanning, MR scanning and other imaging methods became available.
Genetics have advanced with the discovery of the DNA molecule, genetic mapping and gene therapy.
Stem cell research took off in the 2000s (decade), with stem cell therapy as a promising method.
Evidence-based medicine is a modern concept, not introduced to literature until the 1990s.
Prosthetics have improved. In 1958, Arne Larsson in Sweden became the first patient to depend on an artificial cardiac pacemaker. He died in 2001 at age 86, having outlived its inventor, the surgeon, and 26 pacemakers. Lightweight materials as well as neural prosthetics emerged in the end of the 20th century.
Modern surgery
Cardiac surgery was revolutionized in the late 1940s, as open-heart surgery was introduced.
In 1954 Joseph Murray, J. Hartwell Harrison, M.D. and others accomplished the first kidney transplantation. Transplantations of other organs, such as heart, liver and pancreas, were also introduced during the latter 20th century. The first partial face transplant was performed in 2005, and the first full one in 2010. By the end of the 20th century, microtechnology had been used to create tiny robotic devices to assist microsurgery using micro-video and fiber-optic cameras to view internal tissues during surgery with minimally invasive practices.[62]
Laparoscopic surgery was broadly introduced in the 1990s. Natural orifice surgery has followed. Remote surgery is another recent development, with the Lindbergh operation in 2001 as a groundbreaking example.
See also
- Centers for Disease Control and Prevention timeline
- History of pathology
- History of pharmacy
- History of surgery
- Timeline of medicine
References
- ^ Herodotus. "Chapter 77, Book II". The Histories (in English translation).
{{cite book}}: External link in|language= - ^ Nunn, John F. (2002). Ancient Egyptian Medicine. University of Oklahoma Press.
- ^ J. H. Breasted, The Edwin Smith Surgical Papyrus, University of Chicago Press, 1930
- ^ James Henry Breasted, "The Edwin Smith Surgical Papyrus: published in facsimile and hieroglyphic transliteration with translation and commentary in two volumes". (University of Chicago Oriental Institute publications, v. 3-4. Chicago: University of Chicago Press, 1991),9.
- ^ "Edwin Smith papyrus - Britannica Online Encyclopedia". Britannica.com. Retrieved 2012-04-21.
- ^ P. W. Bryan, The Papyrus Ebers, Geoffrey Bles: London, 1930
- ^ Griffith, F. Ll. The Petrie Papyri: Hieratic Papyri from Kahun and Gurob
- ^ "The Kahun Gynaecological Papyrus". Reshafim.org.il. Retrieved 2012-04-21.
- ^ Helaine Selin, Hugh Shapiro, eds., Medicine Across Cultures: History and Practice of Medicine in Non-Western Cultures, Springer 2003, p.35
- ^ a b H. F. J. Horstmanshoff, Marten Stol, Cornelis Tilburg (2004), Magic and Rationality in Ancient Near Eastern and Graeco-Roman Medicine, p. 99, Brill Publishers, ISBN 90-04-13666-5.
- ^ Marten Stol (1993), Epilepsy in Babylonia, p. 55, Brill Publishers, ISBN 90-72371-63-1.
- ^ H. F. J. Horstmanshoff, Marten Stol, Cornelis Tilburg (2004), Magic and Rationality in Ancient Near Eastern and Graeco-Roman Medicine, p. 97-98, Brill Publishers, ISBN 90-04-13666-5.
- ^ Kenneth G. Zysk, Asceticism and Healing in Ancient India: Medicine in the Buddhist Monastery, Oxford University Press, rev. ed. (1998) ISBN 0-19-505956-5
- ^ "Sushruta: The first Plastic Surgeon in 600 B.C." ISPUB. Retrieved 2012-04-21.
- ^ Dominik Wujastyk, ed., The Roots of Ayurveda, Penguin (2003) ISBN 0-14-044824-1
- ^ Arab Medicine during the Ages by Hakim Syed Zillur Rahman, Studies in History of Medicine and Science, IHMMR, New Delhi, Vol. XIV, No. 1-2, 1996, p. 1-39
- ^ Unschuld (2003), 1.
- ^ Sivin (1993).
- ^ "回眸:当年传教士进羊城_MW悦读室之岭南话廊_凤凰网博报- 博采众家之言 报闻公民心声-凤凰网". Blog.ifeng.com. Retrieved 2012-11-03.
- ^ "合信的《全体新论》与广东士林-《广东史志》1999年01期-中国知网". Mall.cnki.net. 2012-02-03. Retrieved 2012-11-03.
- ^ Inasmuch (2010-04-06). "Inasmuch: Mary H. Fulton, The United Study of Forring: 9781140341802: Amazon.com: Books". Amazon.com. Retrieved 2012-11-03.
- ^ http://www.hkbu.edu.hk/~libimage/theses/abstracts/b15564174a.pdf
- ^ "中国近代第一所女子医学院--夏葛医学院-【维普网】-仓储式在线作品出版平台-www.cqvip.com". Cqvip.com. Retrieved 2012-11-03.
- ^ "A crusade of compassion for the healing of the nations: a study of medical ... - Belle Jane Allen, Caroline Atwater Mason - Google Boeken". Books.google.com. Retrieved 2012-11-03.
- ^ "柔济医院的实验室_新闻_腾讯网". News.qq.com. 2012-01-17. Retrieved 2012-11-03.
- ^ Rebecca Chan Chung, Deborah Chung and Cecilia Ng Wong, "Piloted to Serve", 2012
- ^ "Piloted to Serve". Facebook. Retrieved 2012-11-03.
- ^ a b Risse, G. B. (1990). Mending bodies, saving souls: a history of hospitals. Oxford University Press. p. 56.
- ^ a b Askitopoulou, H., Konsolaki, E., Ramoutsaki, I., Anastassaki, E. (2002). "Surgical cures by sleep induction as the Asclepieion of Epidaurus". The history of anesthesia: proceedings of the Fifth International Symposium, by José Carlos Diz, Avelino Franco, Douglas R. Bacon, J. Rupreht, Julián Alvarez. Elsevier Science B.V., International Congress Series 1242. pp. 11–17.
{{cite web}}: CS1 maint: multiple names: authors list (link) - ^ Hippocrates: The "Greek Miracle" in Medicine
- ^ "The Father of Modern Medicine: Hippocrates". Web.archive.org. 2008-02-28. Archived from the original on 2008-02-28. Retrieved 2012-04-21.
- ^ Silverberg, Robert (1967). The dawn of medicine. Putnam. Retrieved 16 January 2013.
- ^ Loudon, Irvine (2002-03-07). Western Medicine: An Illustrated History. Oxford University Press. ISBN 9780199248131. Retrieved 16 January 2013.
- ^ Nutton, Vivian (2012-12-20). Ancient Medicine. Routledge. ISBN 9780415520942. Retrieved 16 January 2013.
- ^ Day, Cyrus L. (1967). Quipus and Witches' Knots. Lawrence, Kansas: University of Kansas Press. pp. 86–89, 124–126.
- ^ Longrigg, James (1993). Greek Rational Medicine: Philosophy and Medicine from Alcmaeon to the Alexandrians. Psychology Press. ISBN 9780415025942. Retrieved 16 January 2013.
- ^ Galen, On the Natural Faculties, Books I, II, and III, Loeb Classical Library, Harvard, 2000
- ^ Mason, A History of the Sciences, p 57
- ^ Dear, Peter. Revolutionizing the Sciences: European Knowledge and Its Ambitions, 1500-1700. Princeton, NJ: Princeton University Press (2001), 37-39.
- ^ "Surgical Instruments from Ancient Rome". Healthsystem.virginia.edu. Retrieved 2012-04-21.
- ^ Roman period surgery set on show, BBC
- ^ William Alexander Greenhill, Chirurgia
- ^ The Romans carried out cataract ops, BBC
- ^ George Sarton, Introduction to the History of Science.
(cf. Dr. A. Zahoor and Dr. Z. Haq (1997), Quotations From Famous Historians of Science, Cyberistan. - ^ Nancy G. Siraisi, " Medicine, 1450–1620, and the History of Science," Isis (2012) 103#3 pp 491-514 DOI: 10.1086/667970
- ^ Michael Servetus Research Website with a graphical study on the Manuscript of Paris by Servetus
- ^ Nancy G. Siraisi, Medieval and Early Renaissance Medicine: An Introduction to Knowledge and Practice (1990) p 21
- ^ Mary Fissell, "The Disappearance of the Patient's Narrative and the Invention of Hospital Medicine," in British Medicine in an Age of Reform ed. by Roger French and Andrew Wear, (1991).
- ^ Guenter B. Risse, Mending Bodies, Saving Souls: A History of Hospitals (1999)
- ^ Madigan M, Martinko J (editors) (2006). Brock Biology of Microorganisms (11th ed.). Prentice Hall. ISBN 0-13-144329-1.
{{cite book}}:|author=has generic name (help) - ^ Brian Abel-Smith, A History of the Nursing Profession (1960)
- ^ Dora B. Weiner and Michael J. Sauter, "The City of Paris and the Rise of Clinical Medicine," Osiris (2003) 18#1 pp 23-42
- ^ George Worthington Adams, Doctors in Blue: The Medical History of the Union Army in the Civil War (1996), excerpt and text search; Glenna R. Schroeder-Lein, The Encyclopedia of Civil War Medicine (2012) excerpt and text search.
- ^ H.H. Cunningham, Doctors in Gray: The Confederate Medical Service (1993) excerpt and text search
- ^ Kenneth Link, "Potomac Fever: The Hazards of Camp Life," Vermont History, (1983) 51#2 pp 69-88
- ^ Mary C. Gillett, The Army Medical Department, 1818-1865 (1987)
- ^ William Quentin Maxwell, Lincoln's Fifth Wheel: The Political History of the U.S. Sanitary Commission (1956)
- ^ Justin Martin, Genius of Place: The Life of Frederick Law Olmsted (2011) pp 178-230
- ^ Eugene E. Roseboom, The Civil War Era, 1850-1873 (1944) p 396
- ^ He also built the New York Public Library
- ^ James H. Cassedy, "Numbering the North's Medical Events: Humanitarianism and Science in Civil War Statistics," Bulletin of the History of Medicine, (1992) 66#2 pp 210-233
- ^ Murray, Joseph E., "The First Successful Organ Transplants in Man", Nobel Lect., 1990, Nobelprize.org., Web, July 7, 2010
Bibliography
- Berridge, Virginia. "Health and Medicine" in The Cambridge Social History of Britain, 1750-1950, vol. 3, Social Agencies and Institutions, edited by F M.L. Thompson, (1990).
- Bynum, W. F. and Roy Porter, eds. Companion Encyclopedia of the History of Medicine (2 vol. 1997); 1840pp; 72 long essays by scholars excerpt and text search
- Bynum, W.F. et al. The Western Medical Tradition: 1800-2000 (2006) excerpt and text search
- Conrad, Lawrence I. et al. The Western Medical Tradition: 800 BC to AD 1800 (1995); excerpt and text search
- Loudon, Irvine, ed. Western Medicine: An Illustrated History (1997) online
- McGrew, Roderick. Encyclopedia of Medical History (1985)
- Porter, Roy (1997). The Greatest Benefit to Mankind: A Medical History of Humanity from Antiquity to the Present. Harper Collins. ISBN 0-00-215173-1.
- Porter, Roy, and Dorothy Porter. In Sickness and in Health: The British Experience, 1650-1850 (1988).
- Porter, Roy, ed. The Cambridge Illustrated History of Medicine (2001) excerpt and text search
- Porter, Roy, ed. The Cambridge History of Medicine (2006); 416pp; excerpt and text search same text without the illustrations
- Porter, Roy. Blood and Guts: A Short History of Medicine (2004) 224pp; excerpt and text search
- Rousseau Rousseau, George S., ed. (2003). Framing and Imagining Disease in Cultural History. Basingstoke: Palgrave Macmillan. ISBN 1-4039-1292-0. With Miranda Gill, David Haycock and Malte Herwig.
- Singer, Charles, and E. Ashworth Underwood. A Short History of Medicine (2nd ed. 1962)
- Siraisi, Nancy G. " Medicine, 1450–1620, and the History of Science," Isis (2012) 103#3 pp 491-514 DOI: 10.1086/667970
- Siraisi, Nancy G. Medieval and Early Renaissance Medicine: An Introduction to Knowledge and Practice (1990) excerpt and text search
- Warner, John Harley, and Janet A. Tighe, eds. Major Problems in the History of American Medicine and Public Health (2006), 560pp; readings in primary and secondary sources excerpt and text search
- Watts, Sheldon. Disease and Medicine in World History (2003), 166pp online
- Weatherall, Miles. In Search of a Cure: A History of Pharmaceutical Discovery (1990), emphasis on antibiotics.
- Wohl, Anthony S. Endangered Lives: Public Health in Victorian Britain (1983).
Primary sources
- Sivin, Nathan (1993). "Huang-ti nei-ching 黃帝內經." In Early Chinese Texts: A Bibliographical Guide, ed. by Michael Loewe: 196-215. Institute for East Asian Studies, University of California, Berkeley.
- Unschuld, Paul U. Huang Di Nei Jing Su Wen: Nature, Knowledge, Imagery in an Ancient Chinese Medical Text. (2003).
External links
- American Association for the History of Medicine,
- Science Museum's History of Medicine Website
- Herbermann, Charles, ed. (1913). . Catholic Encyclopedia. New York: Robert Appleton Company.
- Herbermann, Charles, ed. (1913). . Catholic Encyclopedia. New York: Robert Appleton Company.
- History of Medicine, United States National Library of Medicine
- Directory of History of Medicine Collections
- The history of medicine and surgery as portrayed by various artists
- Medicine @ JewishEncyclopedia.com
- Exhibition of the Vatican Library's Medical Holdings @ The Library of Congress
- Info Britain - History of medicine in the UK
- Wellcome Library History of Medicine
- Digital Clendening Library at the University of Kansas Medical Center
- "MacKinney Collection of Medieval Medical Illustrations"
- The Center for the History of Medicine, Countway Library, Harvard Medical School (includes the Warren Anatomical Museum)
- Medical Heritage Library digital curation collaborative
- Centre for History in Public Health, London School of Hygiene and Tropical Medicine
- "The Practice of Phisick" article phisick.com 13 November 2011
- Michael Servetus Research Website with a graphical study on the Manuscript of Paris by Michael Servetus (1546)
- The Medical Heritage of Medieval Armenia. Its Theoretical and Practical Value in the Light of Modern Science

