Nerve growth factor
Nerve growth factor (NGF) is a neurotrophic factor and neuropeptide primarily involved in the regulation of growth, maintenance, proliferation, and survival of certain target neurons. It is perhaps the prototypical growth factor, in that it was one of the first to be described. Since it was first isolated by Nobel Laureates Rita Levi-Montalcini and Stanley Cohen in 1956, numerous biological processes involving NGF have been identified, two of them being the survival of pancreatic beta cells and the regulation of the immune system.
Structure
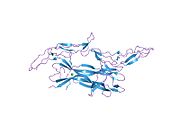
[edit]NGF is initially in a 7S, 130-kDa complex of 3 proteins – Alpha-NGF, Beta-NGF, and Gamma-NGF (2:1:2 ratio) when expressed. This form of NGF is also referred to as proNGF (NGF precursor). The gamma subunit of this complex acts as a serine protease, and cleaves the N-terminal of the beta subunit, thereby activating the protein into functional NGF.
The term nerve growth factor usually refers to the 2.5S, 26-kDa beta subunit of the protein, the only component of the 7S NGF complex that is biologically active (i.e. acting as a signaling molecule).
Function
[edit]As its name suggests, NGF is involved primarily in the growth, as well as the maintenance, proliferation, and survival of nerve cells (neurons) and is critical for the survival and maintenance of sympathetic and sensory neurons as they undergo apoptosis in its absence.[5] However, several recent studies suggest that NGF is also involved in pathways besides those regulating the life cycle of neurons.
Neuronal proliferation
[edit]NGF can drive the expression of genes such as bcl-2 by binding to the Tropomyosin receptor kinase A, which stimulates the proliferation and survival of the target neuron.
High affinity binding between proNGF, sortilin, and p75NTR can result in either survival or programmed cell death. Study results indicate that superior cervical ganglia neurons that express both p75NTR and TrkA die when treated with proNGF,[6] while NGF treatment of these same neurons results in survival and axonal growth. Survival and PCD mechanisms are mediated through adaptor protein binding to the death domain of the p75NTR cytoplasmic tail. Survival occurs when recruited cytoplasmic adaptor proteins facilitate signal transduction through tumor necrosis factor receptor members such as TRAF6, which results in the release of nuclear factor κB (NF-κB) transcription activator.[7] NF-κB regulates nuclear gene transcription to promote cell survival. Alternatively, programmed cell death occurs when TRAF6 and neurotrophin receptor interacting factor (NRIF) are both recruited to activate c-Jun N-terminal kinase (JNK); which phosphorylates c-Jun. The activated transcription factor c-Jun regulates nuclear transcription via AP-1 to increase pro-apoptotic gene transcription.[7]
Proliferation of pancreatic beta cells
[edit]There is evidence that pancreatic beta cells express both the TrkA and p75NTR receptors of NGF. It has been shown that the withdrawal of NGF induces apoptosis in pancreatic beta cells, signifying that NGF may play a critical role in the maintenance and survival of pancreatic beta cells.[8]
Regulation of the immune system
[edit]NGF plays a critical role in the regulation of both innate and acquired immunity. In the process of inflammation, NGF is released in high concentrations by mast cells, and induces axonal outgrowth in nearby nociceptive neurons. This leads to increased pain perception in areas under inflammation. In acquired immunity, NGF is produced by the Thymus as well as CD4+ T cell clones, inducing a cascade of maturation of T cells under infection.[9]
Ovulation
[edit]NGF is abundant in seminal plasma. Recent studies have found that it induces ovulation in some mammals e.g. "induced" ovulators, such as llamas. Surprisingly, research showed that these induced animals will also ovulate when semen from on-schedule or "spontaneous" ovulators, such as cattle is used. Its significance in humans is unknown. It was previously dubbed ovulation-inducing factor (OIF) in semen before it was identified as beta-NGF in 2012.[10]
Mechanism of action
[edit]NGF binds with at least two classes of receptors: the tropomyosin receptor kinase A (TrkA) and low-affinity NGF receptor (LNGFR/p75NTR). Both are associated with neurodegenerative disorders.
When NGF binds to the TrkA receptor, it drives the homodimerization of the receptor, which in turn causes the autophosphorylation of the tyrosine kinase segment.[11] The tropomyosin receptor kinase A receptor has five extracellular domains, and the fifth domain is sufficient in binding NGF.[12] Once bound, the complex undergoes endocytosis and activates the NGF transcriptional program, following two major pathways, the Ras/MAPK pathway and the PI3K/Akt pathway.[11] The binding of NGF to TrkA also leads to the activation of PI 3-kinase, ras, and PLC signaling pathways.[13] Alternatively, the p75NTR receptor can form a heterodimer with TrkA, which has higher affinity and specificity for NGF.
Studies suggest that NGF circulates throughout the entire body via the blood plasma, and is important for the overall maintenance of homeostasis.[14]
Neuron survival
[edit]Binding interaction between NGF and the TrkA receptor facilitates receptor dimerization and tyrosine residue phosphorylation of the cytoplasmic tail by adjacent Trk receptors.[15] Trk receptor phosphorylation sites operate as Shc adaptor protein docking sites, which undergo phosphorylation by the TrkA receptor[7] Once the cytoplasmic adaptor protein (Shc) is phosphorylated by the receptor cytoplasmic tail, cell survival is initiated through several intracellular pathways.
One major pathway leads to the activation of the serine/threonine kinase, Akt. This pathway begins with the Trk receptor complex-recruitment of a second adaptor protein called growth factor-receptor bound protein-2 (Grb2) along with a docking protein called Grb2-associated Binder-1 (GAB1).[7] Subsequently, phosphatidylinositol-3 kinase (PI3K) is activated, resulting in Akt kinase activation.[7] Study results have shown that blocking PI3K or Akt activity results in death of sympathetic neurons in culture, regardless of NGF presence.[16] However, if either kinase is constitutively active, neurons survive even without NGF.[16]
A second pathway contributing to cell survival occurs through activation of the mitogen-activated protein kinase (MAPK) kinase. In this pathway, recruitment of a guanine nucleotide exchange factor by the adaptor and docking proteins leads to activation of a membrane-associated G-protein known as Ras.[7] The guanine nucleotide exchange factor mediates Ras activation through the GDP-GTP exchange process. The active Ras protein phosphorylates several proteins, along with the serine/threonine kinase, Raf.[7] Raf in turn activates the MAPK cascade to facilitate ribosomal s6 kinase (RSK) activation and transcriptional regulation.[7]
Both Akt and RSK, components of the PI3K-Akt and MAPK pathways respectively, act to phosphorylate the cyclic AMP response element binding protein (CREB) transcription factor.[7] Phosphorylated CREB translocates into the nucleus and mediates increased expression of anti-apoptotic proteins,[7] thus promoting NGF-mediated cell survival. However, in the absence of NGF, the expression of pro-apoptotic proteins is increased when the activation of cell death-promoting transcription factors such as c-Jun are not suppressed by the aforementioned NGF-mediated cell survival pathways.[7]
History
[edit]Rita Levi-Montalcini and Stanley Cohen discovered NGF in the 1950s while faculty members at Washington University in St. Louis. The critical discover was done by Levi-Montalcini and Hertha Meyer at the Carlos Chagas Filho Biophysics Institute of the Federal University of Rio de Janeiro in 1952. Their publication in 1954[17] became the definitive proof for the existence of the protein.[18][19] Levi-Montalcini later remarked:
The tumor had given a first hint of its existence in St. Louis but it was in Rio de Janeiro that it revealed itself, and it did so in a theatrical and grand way, as if spurred by the bright atmosphere of that explosive and exhuberant manifestation of life that is the Carnival in Rio.[20]
However, its discovery, along with the discovery of other neurotrophins, was not widely recognized until 1986, when it won the Nobel Prize in Physiology or Medicine.[21][22][23]
Studies in 1971 determined the primary structure of NGF. This eventually led to the discovery of the NGF gene.
NGF is abundant in seminal plasma. Recent studies have found that it induces ovulation in some mammals.[24] Nerve Growth Factors (NGF) were initially discovered due to their actions during development, but NGF are now known to be involved in the function throughout the life of the animal.[25]
Interactions
[edit]Nerve growth factor has been shown to interact with Tropomyosin receptor kinase A.[26]
Clinical Use
[edit]NGF, specifically mouse (murine) nerve growth factor, has been available as a licensed medicine in China since 2003.[27] There is evidence of improved patient outcomes for several diseases of the nervous system, including acute intracerebral hemorrhage,[28] global developmental delay,[29] optic atrophy,[30] epilepsy [31] and cerebral palsy.[32][33] This is significant as there are few medicines which can treat injuries and diseases of the nervous system. Research and clinical use outside of China is limited despite a large body of evidence supporting its use.
Recombinant human nerve growth factor (rhNGF; named cenegermin) has been formulated as an eye drop (0.002%). In 2018 it was approved by the FDA for the treatment of neurotrophic keratitis,[34] a disease in which corneal nerves are damaged or nonfunctional. Without normal corneal sensation, the corneal epithelium does not heal after injury or infection, leading to melting of the corneal stroma and recurrent infections. Clinical trials of cenegermin indicate that the drug can increase the rate of healing of the epithelium.[35][36]
See also
[edit]- Protein targeting
- Nervous system
- VGF Nerve Growth Factor-inducible, a protein whose expression is induced by NGF
- Neurotrophin
- Nerve growth factor receptor
- Growth factor
- Brain-derived neurotrophic factor
References
[edit]- ^ a b c GRCh38: Ensembl release 89: ENSG00000134259 – Ensembl, May 2017
- ^ a b c GRCm38: Ensembl release 89: ENSMUSG00000027859 – Ensembl, May 2017
- ^ "Human PubMed Reference:". National Center for Biotechnology Information, U.S. National Library of Medicine.
- ^ "Mouse PubMed Reference:". National Center for Biotechnology Information, U.S. National Library of Medicine.
- ^ Freeman RS, Burch RL, Crowder RJ, Lomb DJ, Schoell MC, Straub JA, et al. (2004). "NGF deprivation-induced gene expression: After ten years, where do we stand?". NGF and Related Molecules in Health and Disease. Progress in Brain Research. Vol. 146. pp. 111–26. doi:10.1016/S0079-6123(03)46008-1. ISBN 978-0-444-51472-1. PMID 14699960.
- ^ Lee R, Kermani P, Teng KK, Hempstead BL (November 2001). "Regulation of cell survival by secreted proneurotrophins". Science. 294 (5548): 1945–1948. Bibcode:2001Sci...294.1945L. doi:10.1126/science.1065057. PMID 11729324. S2CID 872149.
- ^ a b c d e f g h i j k Sanes DH, Thomas AR, Harris WA (2011). "Naturally-occurring neuron death". Development of the Nervous System, Third Edition. Boston: Academic Press. pp. 171–208. ISBN 978-0-12-374539-2.
- ^ Pierucci D, Cicconi S, Bonini P, Ferrelli F, Pastore D, Matteucci C, et al. (October 2001). "NGF-withdrawal induces apoptosis in pancreatic beta cells in vitro". Diabetologia. 44 (10): 1281–1295. doi:10.1007/s001250100650. PMID 11692177.
{{cite journal}}: CS1 maint: overridden setting (link) - ^ Lambiase A, Bracci-Laudiero L, Bonini S, Bonini S, Starace G, D'Elios MM, et al. (September 1997). "Human CD4+ T cell clones produce and release nerve growth factor and express high-affinity nerve growth factor receptors". The Journal of Allergy and Clinical Immunology. 100 (3): 408–414. doi:10.1016/s0091-6749(97)70256-2. PMID 9314355.
{{cite journal}}: CS1 maint: overridden setting (link) - ^ Ratto MH, Leduc YA, Valderrama XP, van Straaten KE, Delbaere LT, Pierson RA, et al. (September 2012). "The nerve of ovulation-inducing factor in semen". Proceedings of the National Academy of Sciences of the United States of America. 109 (37): 15042–15047. Bibcode:2012PNAS..10915042R. doi:10.1073/pnas.1206273109. PMC 3443178. PMID 22908303.
- Meghan Rosen (August 20, 2012). "Ovulation spurred by newfound semen ingredient". Science News. Archived from the original on 2012-08-24.
- ^ a b Stoleru B, Popescu AM, Tache DE, Neamtu OM, Emami G, Tataranu LG, et al. (March 2013). "Tropomyosin-receptor-kinases signaling in the nervous system". Maedica. 8 (1): 43–48. PMC 3749761. PMID 24023598.
{{cite journal}}: CS1 maint: overridden setting (link) - ^ Wiesmann C, Ultsch MH, Bass SH, de Vos AM (September 1999). "Crystal structure of nerve growth factor in complex with the ligand-binding domain of the TrkA receptor". Nature. 401 (6749): 184–188. Bibcode:1999Natur.401..184W. doi:10.1038/43705. PMID 10490030. S2CID 4337786.
- ^ Marlin MC, Li G (2015). Biogenesis and Function of the NGF/TrkA Signaling Endosome. International Review of Cell and Molecular Biology. Vol. 314. pp. 239–57. doi:10.1016/bs.ircmb.2014.10.002. ISBN 978-0-12-802283-2. PMC 4307610. PMID 25619719.
- ^ Levi-Montalcini R (2004). "The nerve growth factor and the neuroscience chess board". NGF and Related Molecules in Health and Disease. Progress in Brain Research. Vol. 146. pp. 525–27. doi:10.1016/s0079-6123(03)46033-0. ISBN 978-0-444-51472-1. PMID 14699984.
- ^ Kaplan DR, Martin-Zanca D, Parada LF (March 1991). "Tyrosine phosphorylation and tyrosine kinase activity of the trk proto-oncogene product induced by NGF". Nature. 350 (6314): 158–160. Bibcode:1991Natur.350..158K. doi:10.1038/350158a0. PMID 1706478. S2CID 4241996.
- ^ a b Crowder RJ, Freeman RS (April 1998). "Phosphatidylinositol 3-kinase and Akt protein kinase are necessary and sufficient for the survival of nerve growth factor-dependent sympathetic neurons". The Journal of Neuroscience. 18 (8): 2933–2943. doi:10.1523/JNEUROSCI.18-08-02933.1998. PMC 6792598. PMID 9526010.
- ^ Levi-Montalcini R, Meyer H, Hamburger V (January 1954). "In vitro experiments on the effects of mouse sarcomas 180 and 37 on the spinal and sympathetic ganglia of the chick embryo". Cancer Research. 14 (1): 49–57. PMID 13126933. Archived from the original on 2024-01-11. Retrieved 2024-01-11.
- ^ Levi-Montalcini R, Calissano P (June 1979). "The nerve-growth factor". Scientific American. 240 (6): 68–77. Bibcode:1979SciAm.240f..68L. doi:10.1038/scientificamerican0679-68. JSTOR 24965219. PMID 472707. Archived from the original on 2024-01-11. Retrieved 2024-01-11.
- ^ Levi-Montalcini R (November 1998). "The saga of the nerve growth factor". NeuroReport. 9 (16): R71–R83. PMID 9858356. Archived from the original on 2024-01-11. Retrieved 2024-01-11.
- ^ Levi-Montalcini R (September 1987). "The nerve growth factor 35 years later". Science. 237 (4819): 1154–1162. Bibcode:1987Sci...237.1154L. doi:10.1126/science.3306916. PMID 3306916. Archived from the original on 2024-01-11. Retrieved 2024-01-11.
- ^ "The 1986 Nobel Prize in Physiology or Medicine for discoveries of growth factors". Archived from the original on 2008-12-02. Retrieved 2005-11-30.
- ^ Presentation Speech by Professor Kerstin Hall The Nobel Prize in Physiology or Medicine 1986 Archived 2008-10-13 at the Wayback Machine
- ^ "Rita Levi-Montalcini – Nobel Lecture". Archived from the original on 2008-08-28. Retrieved 2005-11-30.
- ^ "Ovulation spurred by newfound semen ingredient". 20 August 2012. Archived from the original on 2021-10-28. Retrieved 2021-10-28.
- ^ Adelman, George. Encyclopedia of Neuroscience . Boston: Birkhhaeuser, 1987. Print.[ISBN missing][page needed]
- ^ Nykjaer A, Lee R, Teng KK, Jansen P, Madsen P, Nielsen MS, et al. (February 2004). "Sortilin is essential for proNGF-induced neuronal cell death". Nature. 427 (6977): 843–848. Bibcode:2004Natur.427..843N. doi:10.1038/nature02319. PMID 14985763. S2CID 4343450.
{{cite journal}}: CS1 maint: overridden setting (link) - ^ Zhao M, Li XY, Xu CY, Zou LP (May 2015). "Efficacy and safety of nerve growth factor for the treatment of neurological diseases: a meta-analysis of 64 randomized controlled trials involving 6,297 patients". Neural Regeneration Research. 10 (5): 819–828. doi:10.4103/1673-5374.156989. PMC 4468778. PMID 26109961.
- ^ An S, Jia Y, Tian Y, Sun J, Wei Y, Yue S, et al. (November 2020). "Mouse nerve growth factor promotes neurological recovery in patients with acute intracerebral hemorrhage: A proof-of-concept study". Journal of the Neurological Sciences. 418: 117069. doi:10.1016/j.jns.2020.117069. PMID 32798840. S2CID 220844712.
{{cite journal}}: CS1 maint: overridden setting (link) - ^ Yuan JJ, Wu D, Wang WW, Duan J, Xu XY, Tang JL (August 2021). "A prospective randomized controlled study on mouse nerve growth factor in the treatment of global developmental delay in children". Zhongguo Dang Dai Er Ke Za Zhi = Chinese Journal of Contemporary Pediatrics (in Chinese). 23 (8): 786–790. doi:10.7499/j.issn.1008-8830.2106042. PMC 8428910. PMID 34511166. Archived from the original on 2023-01-20. Retrieved 2024-02-23.
- ^ Ping L (2022). "鼠神经生长因子在视神经萎缩临床治疗中的应用效果" [Effect of mouse nerve growth factor in the clinical treatment of optic atrophy]. 黑龙江医学 (Heilongjiang Medicine) (in Chinese). 46 (10): 1164–1166+1170. ISSN 1004-5775.
- ^ Li YF, Deng J (2023). "鼠神经生长因子联合左乙拉西坦对局灶性发作型癫痫患儿疾病发作情况及神经细胞因子水平的影响" [Effects of mouse nerve growth factor combined with levetiracetam on seizures and levels of neural cytokines in children with focal onset epilepsy]. 临床医学研究与实践 (in Chinese). 8 (23): 65–68. doi:10.19347/j.cnki.2096-1413.202323017. ISSN 2096-1413.
- ^ Wu J, Lu AD, Zhang LP, Zuo YX, Jia YP (January 2019). "[Study of clinical outcome and prognosis in pediatric core binding factor-acute myeloid leukemia]". Zhonghua Xue Ye Xue Za Zhi = Zhonghua Xueyexue Zazhi (in Chinese). 40 (1): 52–57. doi:10.3760/cma.j.issn.0253-2727.2019.01.010. PMC 7351698. PMID 30704229.
- ^ Zhao H, Feng H, Li X, Pang W (20 August 2019). "注射用鼠神经生长因子联合康复训练治疗脑性瘫痪患儿的临床疗效" [Clinical efficacy of mouse nerve growth factor for injection combined with rehabilitation training in the treatment of children with cerebral palsy]. 中华实用儿科临床杂志 (Chinese Journal of Practical Pediatrics) (in Chinese). 34 (16): 1237–1240. doi:10.3760/cma.j.issn.2095-428X.2019.16.011. ISSN 2095-428X.
- ^ Commissioner Oo (2020-03-24). "FDA approves first drug for neurotrophic keratitis, a rare eye disease". FDA. Retrieved 2024-11-19.
- ^ Bonini S, Lambiase A, Rama P, Sinigaglia F, Allegretti M, Chao W, et al. (November 2018). "Phase II Randomized, Double-Masked, Vehicle-Controlled Trial of Recombinant Human Nerve Growth Factor for Neurotrophic Keratitis". Ophthalmology. 125 (9): 1332–1343. doi:10.1016/j.ophtha.2018.02.022.
- ^ Pflugfelder SC, Massaro-Giordano M, Perez VL, Hamrah P, Deng SX, Espandar L, et al. (January 2020). "Topical Recombinant Human Nerve Growth Factor (Cenegermin) for Neurotrophic Keratopathy". Ophthalmology. 127 (1): 14–26. doi:10.1016/j.ophtha.2019.08.020.
External links
[edit]- Nerve+Growth+Factor at the U.S. National Library of Medicine Medical Subject Headings (MeSH)
- Overview of all the structural information available in the PDB for UniProt: P01138 (Human Beta-nerve growth factor) at the PDBe-KB.
- Overview of all the structural information available in the PDB for UniProt: P01139 (Mouse Beta-nerve growth factor) at the PDBe-KB.