Interleukin 1 beta
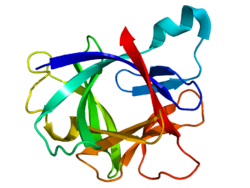
Interleukin-1 beta (IL-1β) also known as leukocytic pyrogen, leukocytic endogenous mediator, mononuclear cell factor, lymphocyte activating factor and other names, is a cytokine protein that in humans is encoded by the IL1B gene.[5][6][7][8] There are two genes for interleukin-1 (IL-1): IL-1 alpha and IL-1 beta (this gene). IL-1β precursor is cleaved by cytosolic caspase 1 (interleukin 1 beta convertase) to form mature IL-1β.
Function
[edit]The fever-producing property of human leukocytic pyrogen (interleukin 1) was purified by Dinarello in 1977 with a specific activity of 10–20 nanograms/kg.[9] In 1979, Dinarello reported that purified human leukocytic pyrogen was the same molecule that was described by Igal Gery in 1972.[10][11][12] He named it lymphocyte-activating factor (LAF) because it was a lymphocyte mitogen. It was not until 1984 that interleukin 1 was discovered to consist of two distinct proteins, now called interleukin-1 alpha and interleukin-1 beta.[6]
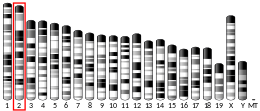
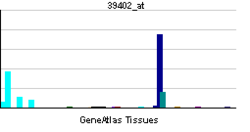
IL-1β is a member of the interleukin 1 family of cytokines. This cytokine is produced by activated macrophages, monocytes, and a subset of dendritic cells known as slanDC,[13] as a proprotein, which is proteolytically processed to its active form by caspase 1 (CASP1/ICE). This cytokine is an important mediator of the inflammatory response, and is involved in a variety of cellular activities, including cell proliferation, differentiation, and apoptosis. The induction of cyclooxygenase-2 (PTGS2/COX2) by this cytokine in the central nervous system (CNS) is found to contribute to inflammatory pain hypersensitivity. This gene and eight other interleukin 1 family genes form a cytokine gene cluster on chromosome 2.[14]
IL-1β, in combination with IL-23, induced expression of IL-17, IL-21 and IL-22 by γδ T cells. This induction of expression is in the absence of additional signals. That suggests IL-1β is involved in modulation of autoimmune inflammation [15]
Different inflammasome complex — cytosolic molecular complex — have been described. Inflammasomes recognize danger signals and activate proinflammatory process and production of IL-1β and IL-18. NLRP3 (contains three domain: pyrin domain, a nucleotide-binding domain and a leucine-rich repeat) type of inflammasome is activated by various stimuli and there are documented several diseases connected to NLRP3 activation like type 2 diabetes mellitus, Alzheimer's disease, obesity and atherosclerosis.[16]
Properties
[edit]Before cleavage by caspase 1, pro-IL-1β has a molecular weight of 37 kDa.[13] The molecular weight of the proteolytically processed IL-1β is 17.5 kDa. IL-1β has the following amino acid sequence:
- APVRSLNCTL RDSQQKSLVM SGPYELKALH LQGQDMEQQV VFSMSFVQGE ESNDKIPVAL GLKEKNLYLS CVLKDDKPTL QLESVDPKNY PKKKMEKRFV FNKIEINNKL EFESAQFPNW YISTSQAENM PVFLGGTKGG QDITDFTMQF VSS
The physiological activity determined from the dose dependent proliferation of murine D10S cells is 2.5 x 108 to 7.1 x 108 units/mg.
IL-1β is present in other species of animals, however non-mammalian sequences of IL-1β lack a conserved cascase-1 cleavage site.[17][18][19]
Clinical significance
[edit]Increased production of IL-1β causes a number of different autoinflammatory syndromes, most notably the monogenic conditions referred to as Cryopyrin-Associated Periodic Syndromes (CAPS), due to mutations in the inflammasome receptor NLRP3 which triggers processing of IL-1β.[20]
Intestinal dysbiosis has been observed to induce osteomyelitis through a IL-1β dependent manner.[21]
The presence of IL-1β has been also found in patients with multiple sclerosis (a chronic autoimmune disease of the central nervous system). However, it is not known exactly which cells produce IL-1β. Treatment of multiple sclerosis with glatiramer acetate or natalizumab has also been shown to reduce the presence of IL-1β or its receptor.[22]
Role in carcinogenesis
[edit]Several types of inflammasomes are suggested to play role in tumorgenesis due to their immunomodulatory properties, modulation of gut microbiota, differentiation and apoptosis. Over-expression of IL-1β caused by inflammasome may result in carcinogenesis. Some data suggest that NLRP3 inflammasome polymorphisms is connected to malignancies such as colon cancer and melanoma. It was reported that IL-1β secretion was elevated in the lung adenocarcinoma cell line A549. It has also been shown in another study that IL-1β, together with IL-8, plays an important role in chemoresistance of malignant pleural mesothelioma by inducing expression of transmembrane transporters.[23] Another study showed that inhibition of inflammasome and IL-1β expression decreased development of cancer cells in melanoma.[24]
Furthermore, it has been found that in breast cancer cells, IL-1β activates p38 and p42/22 MAPK pathways which ultimately lead to the secretion of the RANK/RANKL inhibitor osteoprotegerin. Higher osteoprotegerin and IL-1β levels are a characteristic of breast cancer cells with a higher metastatic potential.[25]
In HIV-1 infections
[edit]The human immunodeficiency virus (HIV) infects cells of the immune system, such as macrophages, dendritic cells, and CD4+ T helper cells (TH). The latter can be infected by the virus in various ways with different fates depending on the state of activation of the T helper cell.[13]
Firstly, TH cells can die of viral lysis due to an active infection that produces enough virions to kill the cell. Secondly, CD4+ T cells can be infected by the virus but instead of producing more viral particles, the cell enters a latent phase. In this period, the T helper cells looks identical from the outside but any stressor could lead to the renewed production of HIV and its propagation to new immune cells. Lastly, the TH cell can become abortively infected, where the virus gets detected inside the cell and a programmed cell-death, known as pyroptosis, kills the infected cell. Pyroptosis is mediated via caspase-1 and is characterized by cell lysis and the secretion of IL-1β causing inflammation and attraction of more immune cells. This can create a cycle of CD4+ T cells getting abortively infect with HIV, dying of pyroptosis, new T helper cells arriving to the site of inflammation where they get infected again. The results is the depletion of T helper cells. Even though, levels of IL-1β in blood are not majorly different between HIV positive and negative individuals, studies have shown elevated levels of IL-1β of lymphatic tissue in HIV-infected individuals.[13]
In fact, the gut-associated lymphoid tissue (GALT) has a high density of immune cells as the gut is an interface between symbiotic gut microbes that should remain with the host and pathogenic bacteria that should not gain access into the circulatory system. If HIV-infection leads to the secretion of IL-1βin monocytes and macrophages, it causes inflammation of this area. The mucosal epithelial layer responds to this by producing less or altering the tight junction proteins which makes it easier for pathogenic microbes to move into the lamina propria. Here, the pathogens can further activate local immune cells and amplify the inflammatory response.[13]
Retinal degeneration
[edit]It has been shown that IL-1 family plays important role in inflammation in many degenerative diseases, such as age-related macular degeneration, diabetic retinopathy and retinitis pigmentosa. Significantly increased protein level of IL-1β has been found in the vitreous of diabetic retinopathy patient. The role of IL-1β has been investigated for potential therapeutic target for treatment of diabetic retinopathy. However, systemic using of canakinumab did not have a significant effect. The role of IL-1β in age-related macular degeneration has not been proven in patient, but in many animal models and in vitro studies it has been demonstrated the role of IL-1β in retinal pigmented epithelial cells and photoreceptor cells damage. NLRP3 inflammasome activate caspase-1 which catalyze cleavage of inactive cytosolic precursor pro-IL-1β to its mature form IL-1β. Retinal pigmented epithelial cells forms blood retinal barrier in human retina which is important for retinal metabolic activity, integrity and inhibition of immune cells infiltration. It has been shown that human retinal pigmented epithelial cells can secrete IL-1 β in exposure to oxidative stress. The inflammatory reaction leads to damage of retinal cells and infiltration of cells of the immune system. The inflammatory process including NLRP3 upregulation is one of the causes of age-related macular degeneration and other retinal diseases that lead to vision loss.[26][27][28] Additionally, it has been shown that caspase-1 is upregulated in the retina of diabetic patients, causing a higher production of IL-1β and subsequent death of retinal neurons.[29]
Neuroinflammation
[edit]Studies in mice on experimental autoimmune encephalomyelitis (EAE), a model for multiple sclerosis (MS) research, have found that blocking IL-1β could make the animals resistant to EAE. IL-1β led to the production of an antigen-specific pro-inflammatory subset of T helper cells (TH17). In combination with other cytokines, interleukin-1β can upregulate the production of the cytokine GM-CSF which is correlated to neuroinflammation. Detailed mechanisms on this front are yet to be elucidated.[29]
IL-1β has also been observed in elevated levels of the cerebrospinal fluid and brain tissues of Alzheimer patients. The amyloid-β plaques, that are characteristic of Alzheimer disease, are damage-associated molecular patterns (DAMPs) that are recognized by pattern recognition receptors (PRRs) and lead to the activation of microglia. Consequently, microglia release interleukin-1β among other cytokines. Nevertheless, the significance of IL-1β in Alzheimer disease and the onset of neuroinflammation still remains largely unknown.[29]
Lastly, in vitro studies have shown that IL-1β causes an increase in mitochondrial glutaminase activity. In response, there is excessive glutamate secretion which has a neurotoxic effect.[29]
As a therapeutic target
[edit]Anakinra is a recombinant and slightly modified version of the human interleukin 1 receptor antagonist protein. Anakinra blocks the biologic activity of IL-1 alpha and beta by competitively inhibiting IL-1 binding to the interleukin type 1 receptor (IL-1RI), which is expressed in a wide variety of tissues and organs. Anakinra is marketed as Kineret and is approved in the US for treatment of RA, NOMID, DIRA.
Canakinumab is a human monoclonal antibody targeted at IL-1B, and approved in many countries for treatment of cryopyrin-associated periodic syndromes.
Rilonacept is an IL-1 trap developed by Regeneron targeting IL-1B, and approved in the US as Arcalyst.[30]
Orthographic note
[edit]Because many authors of scientific manuscripts make the minor error of using a homoglyph, sharp s (ß), instead of beta (β), mentions of "IL-1ß" [sic] often become "IL-1ss" [sic] upon automated transcoding (because ß transcodes to ss). This is why so many mentions of the latter appear in web search results.
References
[edit]- ^ a b c GRCh38: Ensembl release 89: ENSG00000125538 – Ensembl, May 2017
- ^ a b c GRCm38: Ensembl release 89: ENSMUSG00000027398 – Ensembl, May 2017
- ^ "Human PubMed Reference:". National Center for Biotechnology Information, U.S. National Library of Medicine.
- ^ "Mouse PubMed Reference:". National Center for Biotechnology Information, U.S. National Library of Medicine.
- ^ Auron PE, Webb AC, Rosenwasser LJ, Mucci SF, Rich A, Wolff SM, Dinarello CA (December 1984). "Nucleotide sequence of human monocyte interleukin 1 precursor cDNA". Proceedings of the National Academy of Sciences of the United States of America. 81 (24): 7907–7911. Bibcode:1984PNAS...81.7907A. doi:10.1073/pnas.81.24.7907. PMC 392262. PMID 6083565.
- ^ a b "Catabolin" is the name given by Jeremy Saklatvala for IL-1 alpha. March CJ, Mosley B, Larsen A, Cerretti DP, Braedt G, Price V, et al. (1985). "Cloning, sequence and expression of two distinct human interleukin-1 complementary DNAs". Nature. 315 (6021): 641–647. Bibcode:1985Natur.315..641M. doi:10.1038/315641a0. PMID 2989698. S2CID 4240002.
- ^ Clark BD, Collins KL, Gandy MS, Webb AC, Auron PE (October 1986). "Genomic sequence for human prointerleukin 1 beta: possible evolution from a reverse transcribed prointerleukin 1 alpha gene". Nucleic Acids Research. 14 (20): 7897–7914. doi:10.1093/nar/14.20.7897. PMC 311823. PMID 3490654.
- ^ Bensi G, Raugei G, Palla E, Carinci V, Tornese Buonamassa D, Melli M (1987). "Human interleukin-1 beta gene". Gene. 52 (1): 95–101. doi:10.1016/0378-1119(87)90398-2. PMID 2954882.
- ^ Dinarello CA, Renfer L, Wolff SM (October 1977). "Human leukocytic pyrogen: purification and development of a radioimmunoassay". Proceedings of the National Academy of Sciences of the United States of America. 74 (10): 4624–4627. Bibcode:1977PNAS...74.4624D. doi:10.1073/pnas.74.10.4624. PMC 431999. PMID 22079.
- ^ Gery I, Gershon RK, Waksman BH (July 1972). "Potentiation of the T-lymphocyte response to mitogens. I. The responding cell". The Journal of Experimental Medicine. 136 (1): 128–142. doi:10.1084/jem.136.1.128. PMC 2139184. PMID 5033417.
- ^ Gery I, Waksman BH (July 1972). "Potentiation of the T-lymphocyte response to mitogens. II. The cellular source of potentiating mediator(s)". The Journal of Experimental Medicine. 136 (1): 143–155. doi:10.1084/jem.136.1.143. PMC 2139186. PMID 5033418.
- ^ Gery I, Handschumacher RE (March 1974). "Potentiation of the T lymphocyte response to mitogens. III. Properties of the mediator(s) from adherent cells". Cellular Immunology. 11 (1–3): 162–169. doi:10.1016/0008-8749(74)90016-1. PMID 4549027.
- ^ a b c d e Yaseen MM, Abuharfeil NM, Darmani H (January 2023). "The role of IL-1β during human immunodeficiency virus type 1 infection". Reviews in Medical Virology. 33 (1): e2400. doi:10.1002/rmv.2400. PMID 36209388. S2CID 252762935.
- ^ "Entrez Gene: IL1B interleukin 1, beta".
- ^ Sutton CE, Lalor SJ, Sweeney CM, Brereton CF, Lavelle EC, Mills KH (August 2009). "Interleukin-1 and IL-23 induce innate IL-17 production from gammadelta T cells, amplifying Th17 responses and autoimmunity". Immunity. 31 (2): 331–341. doi:10.1016/j.immuni.2009.08.001. hdl:2262/67623. PMID 19682929.
- ^ Abderrazak A, Syrovets T, Couchie D, El Hadri K, Friguet B, Simmet T, Rouis M (April 2015). "NLRP3 inflammasome: from a danger signal sensor to a regulatory node of oxidative stress and inflammatory diseases". Redox Biology. 4: 296–307. doi:10.1016/j.redox.2015.01.008. PMC 4315937. PMID 25625584.
- ^ Pelegrín P, García-Castillo J, Mulero V, Meseguer J (October 2001). "Interleukin-1beta isolated from a marine fish reveals up-regulated expression in macrophages following activation with lipopolysaccharide and lymphokines". Cytokine. 16 (2): 67–72. doi:10.1006/cyto.2001.0949. PMID 11683587.
- ^ Scapigliati G, Buonocore F, Bird S, Zou J, Pelegrin P, Falasca C, et al. (November 2001). "Phylogeny of cytokines: molecular cloning and expression analysis of sea bass Dicentrarchus labrax interleukin-1beta". Fish & Shellfish Immunology. 11 (8): 711–726. doi:10.1006/fsim.2001.0347. PMID 11759041.
- ^ Pelegrín P, Chaves-Pozo E, Mulero V, Meseguer J (March 2004). "Production and mechanism of secretion of interleukin-1beta from the marine fish gilthead seabream". Developmental and Comparative Immunology. 28 (3): 229–237. doi:10.1016/j.dci.2003.08.002. PMID 14642889.
- ^ Masters SL, Simon A, Aksentijevich I, Kastner DL (2009). "Horror autoinflammaticus: the molecular pathophysiology of autoinflammatory disease (*)". Annual Review of Immunology. 27: 621–668. doi:10.1146/annurev.immunol.25.022106.141627. PMC 2996236. PMID 19302049.
- ^ Lukens JR, Gurung P, Vogel P, Johnson GR, Carter RA, McGoldrick DJ, et al. (December 2014). "Dietary modulation of the microbiome affects autoinflammatory disease". Nature. 516 (7530): 246–249. Bibcode:2014Natur.516..246L. doi:10.1038/nature13788. PMC 4268032. PMID 25274309.
- ^ Lin CC, Edelson BT (June 2017). "New Insights into the Role of IL-1β in Experimental Autoimmune Encephalomyelitis and Multiple Sclerosis". Journal of Immunology. 198 (12): 4553–4560. doi:10.4049/jimmunol.1700263. PMC 5509030. PMID 28583987.
- ^ Milosevic V, Kopecka J, Salaroglio IC, Libener R, Napoli F, Izzo S, et al. (January 2020). "Wnt/IL-1β/IL-8 autocrine circuitries control chemoresistance in mesothelioma initiating cells by inducing ABCB5". International Journal of Cancer. 146 (1): 192–207. doi:10.1002/ijc.32419. hdl:2318/1711962. PMID 31107974. S2CID 160014053.
- ^ Moossavi M, Parsamanesh N, Bahrami A, Atkin SL, Sahebkar A (November 2018). "Role of the NLRP3 inflammasome in cancer". Molecular Cancer. 17 (1): 158. doi:10.1186/s12943-018-0900-3. PMC 6240225. PMID 30447690.
- ^ Tulotta C, Ottewell P (July 2018). "The role of IL-1B in breast cancer bone metastasis". Endocrine-Related Cancer. 25 (7): R421–R434. doi:10.1530/ERC-17-0309. PMC 5987176. PMID 29760166.
- ^ Bian ZM, Field MG, Elner SG, Kahlenberg JM, Elner VM (May 2018). "Distinct CD40L receptors mediate inflammasome activation and secretion of IL-1β and MCP-1 in cultured human retinal pigment epithelial cells". Experimental Eye Research. 170: 29–39. doi:10.1016/j.exer.2018.02.014. PMC 5924621. PMID 29454857.
- ^ Tseng WA, Thein T, Kinnunen K, Lashkari K, Gregory MS, D'Amore PA, Ksander BR (January 2013). "NLRP3 inflammasome activation in retinal pigment epithelial cells by lysosomal destabilization: implications for age-related macular degeneration". Investigative Ophthalmology & Visual Science. 54 (1): 110–120. doi:10.1167/iovs.12-10655. PMC 3544415. PMID 23221073.
- ^ Wooff Y, Man SM, Aggio-Bruce R, Natoli R, Fernando N (2019-07-16). "IL-1 Family Members Mediate Cell Death, Inflammation and Angiogenesis in Retinal Degenerative Diseases". Frontiers in Immunology. 10: 1618. doi:10.3389/fimmu.2019.01618. PMC 6646526. PMID 31379825.
- ^ a b c d Mendiola AS, Cardona AE (May 2018). "The IL-1β phenomena in neuroinflammatory diseases". Journal of Neural Transmission. 125 (5): 781–795. doi:10.1007/s00702-017-1732-9. PMC 5699978. PMID 28534174.
- ^ "ARCALYSTTM (rilonacept) Product Label" (PDF). Regeneron Pharmaceuticals, Inc. U.S. Food and Drug Administration. Retrieved 5 October 2020.
Further reading
[edit]- Smirnova MG, Kiselev SL, Gnuchev NV, Birchall JP, Pearson JP (2003). "Role of the pro-inflammatory cytokines tumor necrosis factor-alpha, interleukin-1 beta, interleukin-6 and interleukin-8 in the pathogenesis of the otitis media with effusion". European Cytokine Network. 13 (2): 161–172. PMID 12101072.
- Griffin WS, Mrak RE (August 2002). "Interleukin-1 in the genesis and progression of and risk for development of neuronal degeneration in Alzheimer's disease". Journal of Leukocyte Biology. 72 (2): 233–238. doi:10.1189/jlb.72.2.233. PMC 3835694. PMID 12149413.
- Arend WP (2003). "The balance between IL-1 and IL-1Ra in disease". Cytokine & Growth Factor Reviews. 13 (4–5): 323–340. doi:10.1016/S1359-6101(02)00020-5. PMID 12220547.
- Chakravorty M, Ghosh A, Choudhury A, Santra A, Hembrum J, Roychoudhury S (February 2004). "Ethnic differences in allele distribution for the IL8 and IL1B genes in populations from eastern India". Human Biology. 76 (1): 153–159. doi:10.1353/hub.2004.0016. PMID 15222686. S2CID 2816300.
- Joseph AM, Kumar M, Mitra D (January 2005). "Nef: "necessary and enforcing factor" in HIV infection". Current HIV Research. 3 (1): 87–94. doi:10.2174/1570162052773013. PMID 15638726.
- Maruyama Y, Stenvinkel P, Lindholm B (2005). "Role of interleukin-1beta in the development of malnutrition in chronic renal failure patients". Blood Purification. 23 (4): 275–281. doi:10.1159/000086012. PMID 15925866. S2CID 72570361.
- Milosevic V, Kopecka J, Salaroglio IC, Libener R, Napoli F, Izzo S, et al. (January 2020). "Wnt/IL-1β/IL-8 autocrine circuitries control chemoresistance in mesothelioma initiating cells by inducing ABCB5". International Journal of Cancer. 146 (1): 192–207. doi:10.1002/ijc.32419. hdl:2318/1711962. PMID 31107974. S2CID 160014053.
- Roy D, Sarkar S, Felty Q (January 2006). "Levels of IL-1 beta control stimulatory/inhibitory growth of cancer cells". Frontiers in Bioscience. 11: 889–898. doi:10.2741/1845. PMID 16146780. S2CID 23009646.
- Copeland KF (December 2005). "Modulation of HIV-1 transcription by cytokines and chemokines". Mini Reviews in Medicinal Chemistry. 5 (12): 1093–1101. doi:10.2174/138955705774933383. PMID 16375755.
- Prinz C, Schwendy S, Voland P (September 2006). "H pylori and gastric cancer: shifting the global burden". World Journal of Gastroenterology. 12 (34): 5458–5464. doi:10.3748/wjg.v12.i34.5458. PMC 4088226. PMID 17006981.
- Kamangar F, Cheng C, Abnet CC, Rabkin CS (October 2006). "Interleukin-1B polymorphisms and gastric cancer risk--a meta-analysis". Cancer Epidemiology, Biomarkers & Prevention. 15 (10): 1920–1928. doi:10.1158/1055-9965.EPI-06-0267. PMID 17035400. S2CID 8542733.
External links
[edit]- IL1B+protein,+human at the U.S. National Library of Medicine Medical Subject Headings (MeSH)
This article incorporates text from the United States National Library of Medicine, which is in the public domain.